DEVELOPMENT OF A PATIENT-CENTERED, POST-DISCHARGE VENOUS THROMBOEMBOLISM RISK CALCULATOR FOLLOWING RESECTION FOR COLORECTAL CANCER
Cary Jo Schlick*1, Jessica Y. Liu1,2, Anthony Yang1, David J. Bentrem1, Karl Bilimoria1,2, Ryan P. Merkow1,2
1Surgical Outcomes and Quality Improvement Center, Department of Surgery, Feinberg School of Medicine, Northwestern University, Chicago, IL; 2Division of Research and Optimal Patient Care, American College of Surgeons, Chicago, IL
INTRODUCTION: High-level evidence supports the use of 28 days of venous thromboembolism (VTE) prophylaxis following major abdominal/pelvic resection for cancer to reduce the risk of VTE. However, some studies suggest that not all cancer patients require extended prophylaxis, and tailoring post-discharge VTE prophylaxis to a patient's individual risk may be beneficial. Our objectives were (1) to identify rates of post-discharge VTE in a large cohort of patients following colorectal cancer resection, (2) to identify risk factors associated with post-discharge VTE, and (3) to develop a post-discharge VTE risk calculator to be used at the time of discharge.
METHODS: Patients who underwent colorectal cancer resection from 2012-2016 were identified from ACS NSQIP using procedure targeted variables. Patients were excluded if they suffered an inpatient VTE or death. Post-discharge VTE was defined as pulmonary embolism or deep vein thrombosis diagnosed after the date of discharge from the index hospitalization, but within 30 days of resection. Incorporating pre-, intra- and post-operative variables, a risk calculator designed for use prior to patient discharge was constructed.
RESULTS: Of 51,139 analyzed patients, 387 (0.76%) developed post-discharge VTE. The median time to post-discharge VTE was 11 days (IQR 5-16 days). Preoperative factors associated with post-discharge VTE were race other than white or black (OR 0.55, 95% CI 0.39-0.76 vs. white race), BMI (overweight: OR 1.42, 95% CI 1.07-1.90; obese: OR 1.82, 95% CI 1.34-2.48; morbidly obese: OR 2.25, 95% CI 1.64-3.08 vs. normal weight), and elevated platelet count (>400,000 OR 1.41, 95% CI 1.04-1.92, vs. 150,000-400,000). Intraoperative factors included emergency case classification (OR 1.61, 95% CI 1.11-2.33), operative time (4-6 hours: OR 1.56, 95% CI 1.12-2.18; >6 hours: OR 1.86, 95% CI 1.21-2.84, vs. <2 hours), and type of operation (laparoscopic partial colectomy: OR 0.60, 95% CI 0.46-0.77; open proctectomy: OR 0.55, 95% CI 0.37-0.80; and laparoscopic proctectomy: OR 0.43, 95% CI 0.30-0.61, vs. open partial colectomy). Postoperative factors included anastomotic leak (OR 2.04, 95% CI 1.30-3.19) and ileus (OR 1.38, 95% CI 1.07-1.78). The predicted probability of post-discharge VTE from the derivation cohort ranged from 0.04% to 10.21% depending on the patient's specific risk (Figure 1). The calculator's C-statistic was 0.68, and the calibration was good (p=0.120).
CONCLUSION: Patient-specific characteristics are associated with varying rates of post-discharge VTE. We present the first multi-institutional post-discharge VTE risk calculator designed for use at the time of discharge following colorectal cancer resection. This tool can be used to counsel patients regarding the importance of post-discharge VTE prophylaxis and to tailor extended VTE chemoprophylaxis recommendations to individual patients.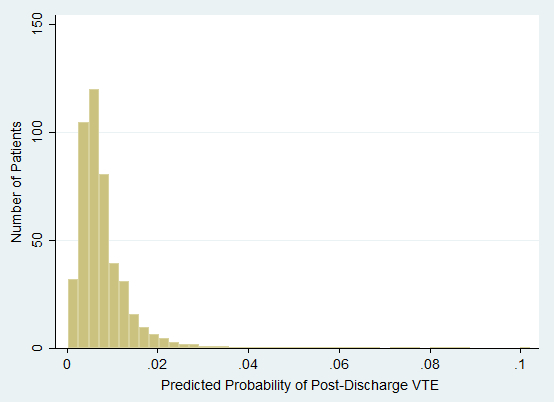
Figure 1: Predicted probability of post-discharge VTE following colorectal cancer resection in risk calculator derivation cohort.
Back to 2019 Abstracts




