ROLE OF ENDOSCOPIC RESECTION VERSUS SURGICAL RESECTION IN MANAGEMENT OF MALIGNANT COLON POLYPS: A NATIONAL CANCER DATABASE ANALYSIS
Dhruv Lowe*1, Shreya Sinha2, Sheikh A Saleem1, Gary Brooks3, Muhammad Arif1
1Gastroenterology, SUNY Upstate Medical University, Syracuse, NY; 2Hematology Oncology, SUNY Upstate Medical University, Syracuse, NY; 3Public Health and Preventive Medicine, SUNY Upstate Medical University, Syracuse, NY
BACKGROUND: The overall incidence and mortality from colon cancer has decreased over the last three decades. This is attributed to nationwide surveillance programs and timely removal of colon polyps. Although mostly benign, 2 to 5% of polyps removed endoscopically can harbor invasive malignancy. Post polypectomy management of such polyps has been controversial. Surgical resection (SR) or observation after initial endoscopic resection (ER) are the two main approaches. There are very few large population-based studies comparing outcomes and utilization trends of these two approaches in an American cohort and none over the last decade.
METHODS: Using the National Cancer Database, we identified patients ≥18 years with a diagnosis of T1N0M0 invasive colon adenocarcinoma from 2004 to 2015. Only patients with a negative residual tumor margin were included. Patients were further categorized as SR or ER depending on the most invasive intervention. Primary outcome was the overall survival (OS) compared using Kaplan Meier curves. Cox proportional hazards regression analysis was performed to evaluate independent factors affecting overall survival. Factors predicting utilization were assessed using logistic regression and Pearson's chi-squared test.
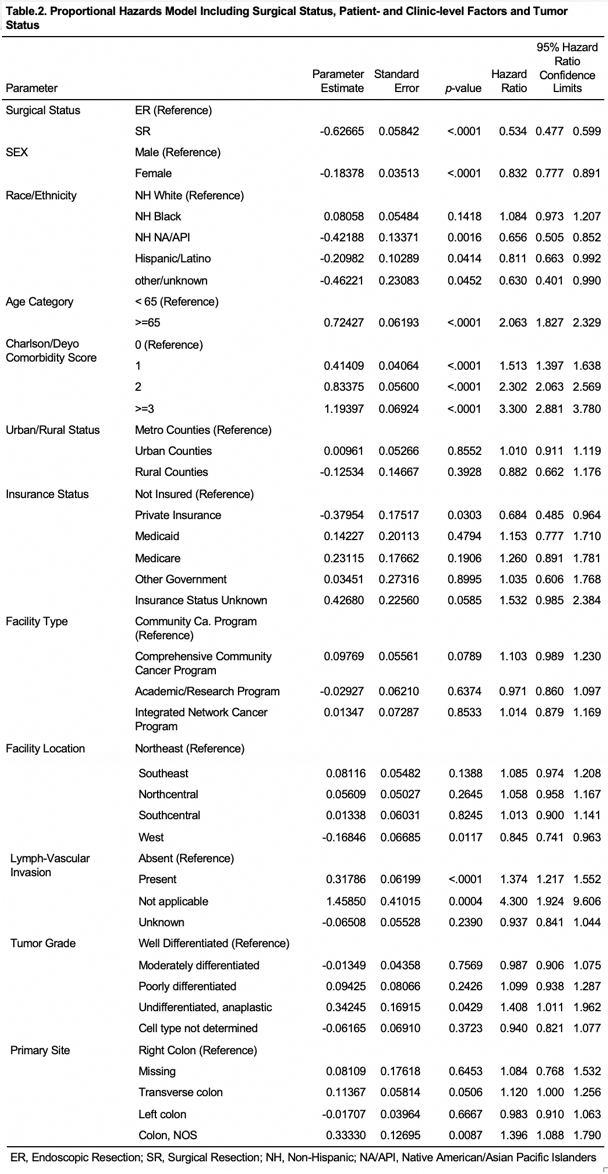
RESULTS: Out of a possible 832638 patients in the data set, 40435 met the inclusions criteria. 91.6 % patients underwent SR and 8.4% underwent ER. Median age for SR was 68 years and for ER was 66 years. Median follow up was 3.8 years for SR and 3.3 years for ER (P <.0001). Factors affecting utilization of endoscopic resection versus surgical resection are shown in Table 1. Patients less than 65 years, non-White race, male gender, Charlson score of 0 or ≥3, Medicaid or uninsured patients, left colonic and well differentiated polyps were factors associated with a proportionally higher use of ER. Overall survival was significantly better in the surgical group compared to the polypectomy group. 1-year and 5-year survival for SR were 94.8% and 83.6% respectively compared to 92.1% and 76.6% for ER (P <.0001). The adjusted Hazard ratio for SR was 0.534 (p <.0001). Independent factors favoring overall survival included female sex, Hispanics/Native Americans, younger age, Charlson score 0, absence of lymphovascular invasion, and private health insurance (Table 2). Patients who underwent ER had lower 30-day mortality [Relative risk for ER = 0.52 (95% CI= 0.35-0.76)][GSB4] but there was no difference in 90-day mortality [Relative risk for ER = 1.05 (95% CI=0.84-1.30)].
CONCLUSION: Our study is the largest population-based analysis of patients with T1N0M0 malignant colon polyp, comparing outcomes between SR and ER. Overall survival was higher in patients who underwent surgical resection compared to endoscopic resection. This remained consistent even after adjusting for multiple patient and tumor factors between the two groups.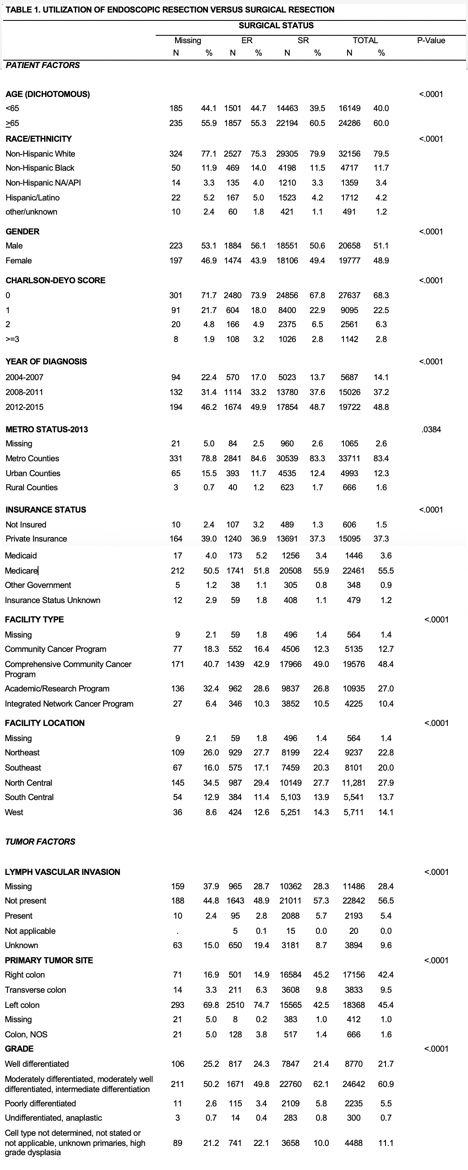
Back to 2019 Abstracts




