PERIOPERATIVE MORTALITY AND MORBIDITY AMONG 8,193 PATIENTS WITH CIRRHOSIS UNDERGOING EMERGENT VERSUS NON-EMERGENT ABDOMINAL SURGERY IN A NATIONAL HEALTHCARE SYSTEM
Kira L. Newman*1, Kay Johnson2, Paul Cornia2, Kristin Wyatt2, Pamela Green2, Peter Wu2,3, George N. Ioannou1,2
1Medicine, University of Washington, Seattle, WA; 2VA Puget Sound Health Care System, Seattle, WA; 3Surgery, University of Washington, Seattle, WA
Background: Perioperative morbidity and mortality are higher in patients with cirrhosis compared to non-cirrhotic patients. As a result, surgeons may be reluctant to operate on cirrhotic patients, even when they are well-compensated. However, few studies have documented the risk of emergent surgery compared to non-emergent procedures among cirrhotic patients. We aimed to compare 30-day mortality and morbidity and risk factors for poor outcomes following emergent versus non-emergent abdominal surgery in a large sample of cirrhotic patients.
Methods: We analyzed data from the national Veterans Affairs Surgical Quality Improvement Program (VASQIP), which is a national prospective surgical outcomes database established by the Veterans Administration in 1991. We identified 8,193 patients with cirrhosis who underwent 9,259 abdominal surgeries between 2001 and 2017 and compared outcomes of emergent procedures versus non-emergent surgeries, after adjusting for type of surgery, age, sex, race/ethnicity, diabetes, etiology of cirrhosis, functional status, congestive heart failure, severe COPD, and dialysis.
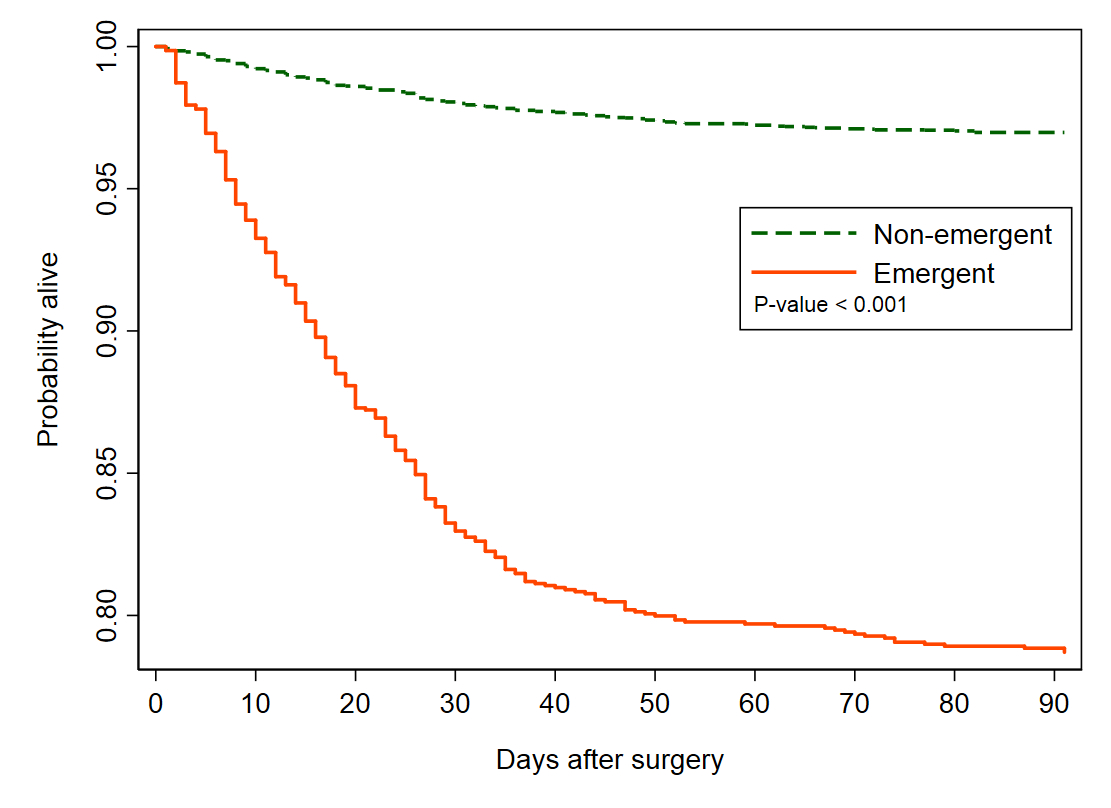
Results: Of the 9,259 abdominal surgical procedures, 7,850 (84.8%) were non-emergent and 1,409 (15.2%) were emergent. The most common abdominal surgeries included were hernia repairs (50.8%) and cholecystectomies (20.7%). Compared to non-emergent surgeries, emergent surgeries had higher 30-day mortality (17.2% vs 2.1%, adjusted odds ratio [AOR] 5.88 95% CI 4.76-7.69), higher 90-day mortality (21.3% vs 3.0%, AOR 5.56 95% CI 4.55-6.67), higher risk of a surgical complications (33.1% vs 12.5%, AOR 2.78 95% CI 2.38-3.23) and longer length of hospital stay (days) (11.5 vs 4.6, adjusted incident-rate ratio 2.63 95% CI 2.44-2.86). After adjustment for potential confounders, risk factors for mortality among cirrhotic patients undergoing non-emergent and emergent surgeries were similar, with decreased functional status, presence of ascites, presence of gastroesophageal varices, high MELD score, and need for intraoperative blood transfusion all significantly associated with 30-day mortality in both groups. In both groups, colorectal procedures were the highest risk category.
Conclusion: For patients with cirrhosis, emergent surgery is associated with -a nearly six-fold higher mortality than non-emergent surgery. Deferral of procedures in well-managed and stable cirrhotic patients may lead to worse outcomes in the future if a surgery becomes urgently indicated.
Demographic, comorbidity, and surgical risk factors for 30-day post-operative mortality following abdominal surgery in patients with cirrhosis
| Variable | Subcategory | Non-Emergent Surgery N=7,850 | Emergent Surgery N=1409 | ||
| 30-day Mortality N (%) | Adjusted* Odds Ratio | 30-day Mortality N (%) | Adjusted* Odds Ratio | ||
| Age, yrs | ≤ 53 (ref.) | 27 (1.5) | 1 | 33 (11.3) | 1 |
| 53-59 | 42 (1.9) | 1.05 (0.63-1.77) | 56 (15.1) | 1.40 (0.85-2.29) | |
| 59-66 | 44 (2.1) | 0.99 (0.60-1.64) | 60 (15.8) | 1.25 (0.77-2.05) | |
| > 66 | 48 (2.8) | 1.10 (0.67-1.80) | 94 (25.8) | 1.97 (1.21-3.19) | |
| BMI, kg/m2 | BMI < 18.5 (%) | 7 (5.5) | 2.31 (0.92-5.81) | 12 (25.0) | 1.35 (0.57-3.20) |
| BMI 18.5-24.9 (%) (ref.) | 29 (1.6) | 1 | 66 (18.1) | 1 | |
| BMI 25-29.9 (%) | 30 (1.4) | 0.93 (0.54-1.58) | 47 (14.5) | 0.75 (0.47-1.20) | |
| BMI ≥ 30 (%) | 30 (1.6) | 0.99 (0.56-1.75) | 32 (10.8) | 0.58 (0.35-0.98) | |
| Ascites | No (ref.) | 101 (1.5) | 1 | 88 (11.9) | 1 |
| Yes | 60 (5.4) | 4.45 (2.94-6.72) | 155 (23.3) | 2.73 (1.94-3.84) | |
| Gastroesophageal varices | No (ref.) | 101 (1.6) | 1 | 145 (14.1) | 1 |
| Yes | 30 (3.7) | 2.67 (1.63-4.37) | 56 (23.9) | 2.59 (1.73-3.88) | |
| Functional status | Independent (ref.) | 128 (1.7) | 1 | 140 (12.7) | 1 |
| Partially dependent | 21 (6.6) | 3.01 (1.77-5.12) | 52 (26.4) | 2.23 (1.51-3.28) | |
| Totally dependent | 12 (25.5) | 8.29 (3.58-19.23) | 51 (47.7) | 3.82 (2.41-6.08) | |
| MELD score | ≤ 8 (ref.) | 9 (0.7) | 1 | 3 (6.4) | 1 |
| 9-10 | 21 (1.6) | 2.41 (1.09-5.33) | 8 (8.3) | 1.30 (0.31-5.41) | |
| 11-14 | 37 (2.1) | 3.40 (1.63-7.08) | 24 (8.3) | 1.23 (0.33-4.56) | |
| > 14 | 49 (4.4) | 8.86 (4.20-18.68) | 158 (23.1) | 4.71 (1.34-16.62) | |
| Type of abdominal surgery | Hernia repair (ref.) | 34 (0.8) | 1 | 78 (11.9) | 1 |
| Cholecystectomy | 16 (0.9) | 1.07 (0.59-1.95) | 8 (5.6) | 0.41 (0.20-0.87) | |
| Gastric, pancreas, appendectomy | 15 (4.1) | 4.23 (2.23-8.03) | 35 (17.7) | 1.37 (0.87-2.15) | |
| Small bowel, spleen, esophagus | 43 (6.0) | 7.43 (4.59-12.03) | 39 (23.6) | 1.57 (0.96-2.58) | |
| Colorectal | 52 (7.0) | 7.54 (4.78-11.88) | 81 (35.4) | 2.78 (1.87-4.14) | |
| Ileostomy, enterostomy, other | 1 (0.5) | 0.56 (0.08-4.01) | 2 (10.5) | 0.59 (0.11-3.23) | |
| Intraoperative units of red blood cells | 0 (ref.) | 106 (1.4) | 1 | 144 (12.1) | 1 |
| ≥ 1 | 55 (11.3) | 3.52 (2.30-5.38) | 99 (45.2) | 3.82 (2.65-5.53) | |
Ref.=referent group. *Adjusted for type of surgery, age, gender, race/ethnicity, diabetes, etiology of cirrhosis, functional status, CHF, severe COPD, dialysis.
Back to 2019 Abstracts




