|
 |
Back to 2014 Annual Meeting Posters
Population-Based Trends of Pancreaticoduodenectomy: Temporal and Age-Related Outcomes
Cheguevara Afaneh*1, Paul O'Mahoney1, Gregory Giambrone2, Jonathan Eskreis-Winkler2, Akshay U. Bhat3, Ramin Zabih3, Fabrizio Michelassi1, Peter Fleischut2
1Surgery, NY Presbyterian Hospital, New York, NY; 2Anesthesiology, NY Presbyterian Hospital, New York, NY; 3Cornell University, Ithaca, NY
Introduction: Pancreaticoduodenectomy (PD) remains a technically challenging procedure with significant morbidity and mortality. Medical and technological advancements have lead to an ageing patient-population and advanced disease associated with increasing technical challenges and taxing postoperative management. We report outcomes of PD across three major states over a 6-year period.
Methods: Using the State Inpatient Databases (SID), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality, we retrospectively reviewed the outcomes of all PDs performed from 2006 to 2011 in the states of California, Florida, and New York. Patient variables of interest included gender, age distribution, admission & disposition stratification, and payer distribution. Primary end-points included mortality and length of stay (LOS).
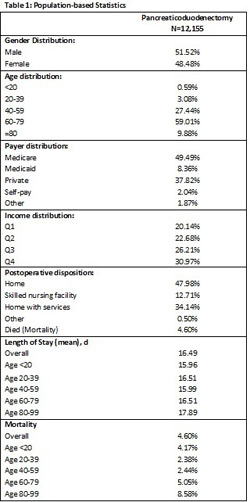
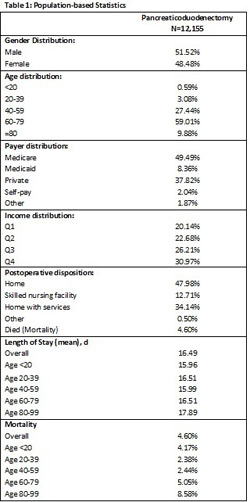
Results: A total of 12,270 PDs were performed in this time period; approximate percent of PDs performed by year were 15% in 2006, 15% in 2007, 16% in 2008, 17% in 2009, 18% in 2010, and 19% in 2011. The majority of patients were male (51.5%), between the ages of 60 and 79 (59.01%), admitted from home (59.97%), received Medicare (49.49%) and discharged home (47.98%) postoperatively (Table 1). The most common indication for PD was a malignant neoplasm of the head of pancreas (46.76%) followed by malignant neoplasm of the Ampulla of Vater (10.54%). Approximately 31.37% of patients required transfusion of packed red blood cells and 16.14% of patients required parenteral nutrition perioperatively. The frequency of percutaneous drainage of an abdominal collection was 7.82%. Approximately 4.82% of patients required continuous invasive mechanical ventilation for ≥96 hours. The proportion of gastroparesis and glucose dysregulation were 2.49% and 1.87%, respectively. Mortality rates and LOS increased with increasing age (Figure 1A). Patients aged 40-59 years had a mortality rate and LOS of 2.44% and 15.99 days, respectively, compared to patients aged ≥80 years who had rates of 8.58% and 17.89 days, respectively. Mortality peaked in 2008 to 5.53%; however, have subsequently decreased over the last three years (3.45% in 2011; Figure 1B). LOS has steadily decreased over the last 5 years, with the lowest LOS in 2011 at 15.12 days (Figure 1B).
Conclusion: Mortality rates and LOS continue to improve following pancreaticoduodenectomy despite an increasingly ageing patient population. Mortality rates and LOS remain lowest for younger patients. The SID has important limitations; therefore, further analyses are necessary to identify the full impact of these findings.

Back to 2014 Annual Meeting Posters
|