|
Back to 2014 Annual Meeting Posters
Quantifying the Burden of Perioperative Complications Following Total Pancreatectomy Using the Postoperative Morbidity Index: a Multi-Institutional Perspective
Jashodeep Datta*1, Russell S. Lewis1, Steven M. Strasberg2, Bruce L. Hall2, Charles M. Vollmer1, Study Group the Pmi1
1Surgery, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA; 2Surgery, Washington University in St. Louis, St. Louis, MO
BACKGROUND: Historically, total pancreatectomy (TP) has been regarded as particularly morbid. While contemporary studies indicate decreasing complication rates following TP, none have quantitatively evaluated the impact of its complications. The Postoperative Morbidity Index (PMI) - a validated measure of complication burden - combines data accrued using ACS-NSQIP criteria with severity weighting derived from the Modified Accordion Grading System. We aimed to establish the perioperative morbidity burden for TP using PMI in a multi-institutional cohort.
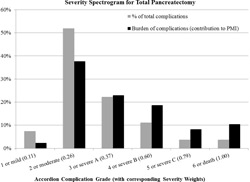
METHODS: Nine institutions contributed data for 64 TPs from 2005-2011. Each NSQIP complication was assigned an Accordion grade with an associated severity weight ranging from 0.110 (grade 1/mild) to 1.00 (grade 6/death). PMI equals the sum of severity weights for all highest-grade complications (Total Burden) divided by total number of patients. It can range along the utility scale from 0 (no complication in any patient) to 1.00 (all patients died of complications). Prior work has established the PMIs of proximal and distal pancreatectomy as 0.115 & 0.087. A severity profile spectrogram was generated to depict the relationship between frequency and burden of complications at each severity grade. Correlates to PMI were determined by regression analysis.
RESULTS: Median age was 65 yrs (range 23-85); the most common indication was pancreatic adenocarcinoma (37.5%). Overall, 29 patients (45.3%) suffered a total of 55 NSQIP complications; 15 (23.4%) had >1 complication. Median length of stay was 10 days. Thirteen patients (20.3%) were readmitted and one death (1.6%) occurred within 30 days. Non-risk adjusted PMI for TP was 0.151, while average burden for the 29 complication-bearing cases rose to 0.333. The most common highest-grade complications were bleeding/transfusion (17.2%) and sepsis (12.5%). Accordion grade 2 complications predominated in frequency (51.9%). Severity spectrogram analysis illustrated discordance between frequency and burden of complications (Figure). Notably, grades 4-6 comprised only 18.5% of complications but contributed 37.1% to the series' Total Burden. Of the 22 standardized NSQIP complications, Organ Space SSI provided a quarter of the Total Burden. On univariate analysis, advanced age (p=0.002), low preoperative sodium level (p=0.03), postoperative bile leak (p=0.04), and length of stay (p<0.001) correlated with PMI.
CONCLUSION: This first multi-institutional series on TP for all indications quantifies the complication burden following TP using the rigor of ACS-NSQIP. A PMI of 0.151 indicates that, collectively, patients undergoing TP have an average burden of complications in the mild severity range (=0.110), underscoring a steadily improving morbidity profile following TP. However, those patients who do develop complications have a substantial reduction in health utility.
Back to 2014 Annual Meeting Posters
|