|
Back to 2014 Annual Meeting Posters
Defining Perioperative Risk After Hepatectomy Based on Diagnosis and Resection Extent
Christopher R. Shubert*1, Michael L. Kendrick1, Kristine Thomsen2, Mark J. Truty1, David M. Nagorney1, Elizabeth B. Habermann2
1Surgery, Mayo Clinic, Rochester, MN; 2Health Care Policy and Research, Surgical Outcomes Program, Mayo Clinic, Rochester, MN
Introduction:
Hepatectomy outcomes are incompletely and inaccurately represented in the current literature, which have not compared outcomes stratified by both extent of resection and diagnosis. We hypothesized that operative risk can be better assessed by stratifying diagnoses into low and high risk categories and extent of resection into major and minor resection categories for more accurate identification of patient outcomes following hepatectomy.
Methods:
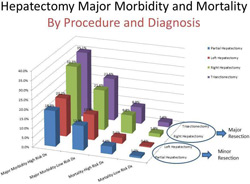
ACS-NSQIP was reviewed for thirty-day operative mortality and major morbidity after Partial Hepatectomy (PH), Left Hepatectomy (LH), Right Hepatectomy (RH), and Trisectionectomy (TS). Mortality was reviewed per diagnosis and "High Risk" was defined as the diagnoses associated with the greatest mortality. Univariate analysis of operative outcomes by resection extent was performed to define "Major" and "Minor" resections. Chi-square, t-tests and multivariable logistic regression were utilized to compare outcomes across groups.
Results:
Within 7,895 patients the highest mortality was observed in Hepatocellular carcinoma (5.2%) and cholangiocarcinoma (8.4%), either intra- or extrahepatic, which were classified as "High Risk". Metastatic disease, benign neoplasms, and gallbladder cancer, experienced mortality of 1.4%, 0.5%, and 1.2% respectively, and were classified as "Low Risk".
PH and LH were statistically similar with respect to operative mortality and major morbidity within respective diagnosis risk groups (Low Risk: PH vs LH and High Risk: PH vs LL; all p>0.31) and were defined as "Minor Resections". Similarly RH and TS had similar rates of operative mortality and major morbidity within respective diagnosis risk groups (Low Risk: RH vs TS and High Risk: RH vs TS; all p>0.43) and were defined as "Major Resections".
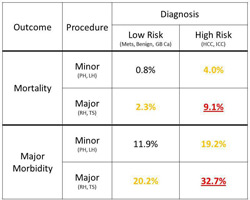
Risks of major morbidity and mortality increased across all diagnosis and the extent of resection groups. Of Minor Resections, High Risk diagnoses had 5 times the mortality and 1.6 times the major morbidity as Low Risk diagnoses. Of Major Resections, High Risk diagnoses had 4 times the mortality and 1.6 times the major morbidity as Low Risk diagnoses. Of Low Risk diagnoses, Major Resections had 2.9 times the mortality and 1.7 times the major morbidity as Minor Resections. Of High Risk diagnoses, Major Resections had 2.3 times the mortality and 1.7 times the major morbidity as Minor Resections. (all p<0.01)
Within both Major and Minor Resections, High Risk diagnosis was an independent risk factor for Mortality (ORs=3.1-3.2) and Major Morbidity (ORs=1.4-1.5).
Conclusion:
Risk of hepatectomy can be better assessed when stratified by both risk of diagnosis and extent of resection, allowing for a more accurate assessment of patient outcomes. These results have significant implications for pre-operative planning, informed consent, resource utilization, and comparisons between centers.
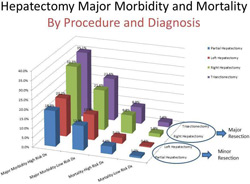
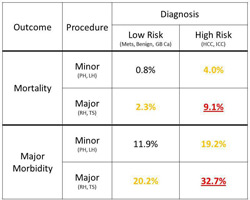 Major Morbidityand Mortality Stratified by Diagnosis Risk Group and by Major and Minor Hepatectomy.
Back to 2014 Annual Meeting Posters
|