|
Back to 2014 Annual Meeting Posters
Flaps for Large Radiated Perineal Wounds After Proctectomy
Somjade J. Songcharoen*, Anna K. Pavlov, Kevin Randolph, Christopher J. Lahr, Peter B. Arnold, Thomas S. Helling
Surgery, Univ Mississippi, Jackson, MS
Background: The increased use of preoperative radiation therapy for low rectal and anal cancers presents the surgeon with large perineal defects that are known to result in poor wound healing. We present 37 cases of flap closure of the radiated perineum following proctectomy for malignancy.
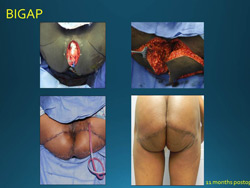
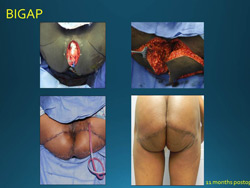
Methods: Thirty-three bilateral (BIGAP) or unilateral (IGAP) fasciocutaneous flaps based on the inferior gluteal perforator artery and four vertical rectus abdominis myocutaneous (VRAM) flaps are included in this study along with associated major and minor complications involving the perineal flaps. VRAM flaps were utilized for relatively large defects or those extensively involving the posterior vaginal wall; otherwise BIGAP flaps were used.
The BIGAP flap technique uses bilateral equilateral triangular incisions of gluteal skin, subcutaneous fat, and gluteal fascia. The dissection of the flaps does not include the muscle, allowing the flaps to slide medially. Damage to the vessels of the pedicle is avoided because the dissection is not carried into the gluteal muscle. The medial side of each triangle is created by the lateral edge of the proctectomy perineal defect and is parallel to the midline of the body. The pelvic defect is filled in by excising a 2 cm vertical strip of skin from the medial side of each triangle. The lateral defect in the gluteal skin is closed in a horizontal V-Y fashion. The center of each equilateral triangle is located above the inferior gluteal artery location.
Results: Defects closed in the BIGAP group ranged from 60 cm3 to 3375 cm3 with a mean of 617 cm3 while defects in the VRAM group ranged from 250 cm3 to 5040 cm3 with a mean of 1676 cm3. Average tumor size was 7.1 cm for both groups. There were no mortalities and no flaps were lost. All perineal wounds healed primarily. Major complications involving the perineum occurred in 21% and 75% of patients receiving BIGAP and VRAM closures, respectively. Minor perineal complications occurred in 61% and 25% respectively.
Conclusion: When local tumor invasion requires the creation of a large defect to remove the tumor in an irradiated field, the use of vascularized flaps reduce the risk of failed wound healing often associated with primary closure.
Back to 2014 Annual Meeting Posters
|