|
Back to 2014 Annual Meeting Posters
Laparoscopic Surgery for Sigmoid Diverticulitis Complicated by Vesical/Vaginal Fistulas
Faisel Elagili*, Emre Gorgun, Meagan Costedio, Feza H. Remzi, Hermann P. Kessler
Colorectal surgery, Cleveland clinic, Cleveland, OH
Background: There are hardly any data on laparoscopic surgery for sigmoid diverticulitis complicated by entero-vesical and -vaginal fistulas. The aim of our study was to evaluate feasibility and outcomes of such patients.
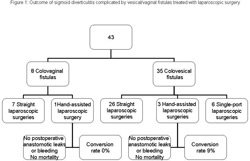
Patients and methods: Data of patients undergoing laparoscopic surgery for diverticular disease with fistulas between 2004 and 2013 were obtained from our prospective IRB approved database. Short term outcomes were evaluated. Results: 43 patients (60% male) were recruited; diagnosis was colovesical fistula in 35 patients and colovaginal fistula in 8 patients, the median age was 60 (28-84) years, mean body mass index was 28.2 ± 5.5; 51% of patients were ASA grade II. Diverticular colovesical fistulas were managed by sigmoid resection alone (n=21) or in combination with suture repair of the bladder (n=5), partial cystectomy (n=1), omental pedicle graft (n=4), as Hartmann's procedure (n=1), left colectomy (n=1) or with low anterior resection (n=2).
The colovaginal fistulas were managed by sigmoid resection (n=6), eventually with omentoplasty (n=1), one patient required additional suture repair of fistula.
The median operative time was 180 (34-319) min; the median estimated blood loss was 100 (25-600) ml. The median hospital stay was 5 (1-22) days (5 [1-22] days in non-converted vs. 7 [4-8] days in converted cases). 3 (7%) patients required conversion; the reasons were dense adhesions (n=1), difficult mobilization of the rectum in the low pelvis (n=1) and associated hiatal hernia with transverse colon being prolapsed (n=1). In 5 patients, a mini laparotomy was needed for fistula management: one patient tolerated the pneumoperitoneum poorly, in 3 patients the fistula was difficult to dissect laparoscopically and in one patient a large phlegmon was present.
The conversion rate was 9 % (3/35) for the bladder fistulas and 0% for the vaginal fistulas, there were no major intraoperative complication, no postoperative anastomotic leaks or bleeding and no mortality.
There were 9 minor complications (21%), including postoperative ileus (n=4), wound infection (n=1), urinary tract infection (n=3) and deep venous thrombosis (n=1).
Conclusion: Laparoscopic surgery of sigmoid diverticulitis complicated by entero-vesical and -vaginal fistula is feasible and safe; this approach offers short hospitalization like in uncomplicated cases and favorable short term outcome
Back to 2014 Annual Meeting Posters
|