|
|
Back to Annual Meeting Posters Effect of Instrument Type on Transanal Endoscopic Microsurgery (TEM) Learning Curves Ezra N. Teitelbaum*, Fahd O. Arafat, Brittany Lapin, Anne M. Boller Northwestern University, Chicago, IL
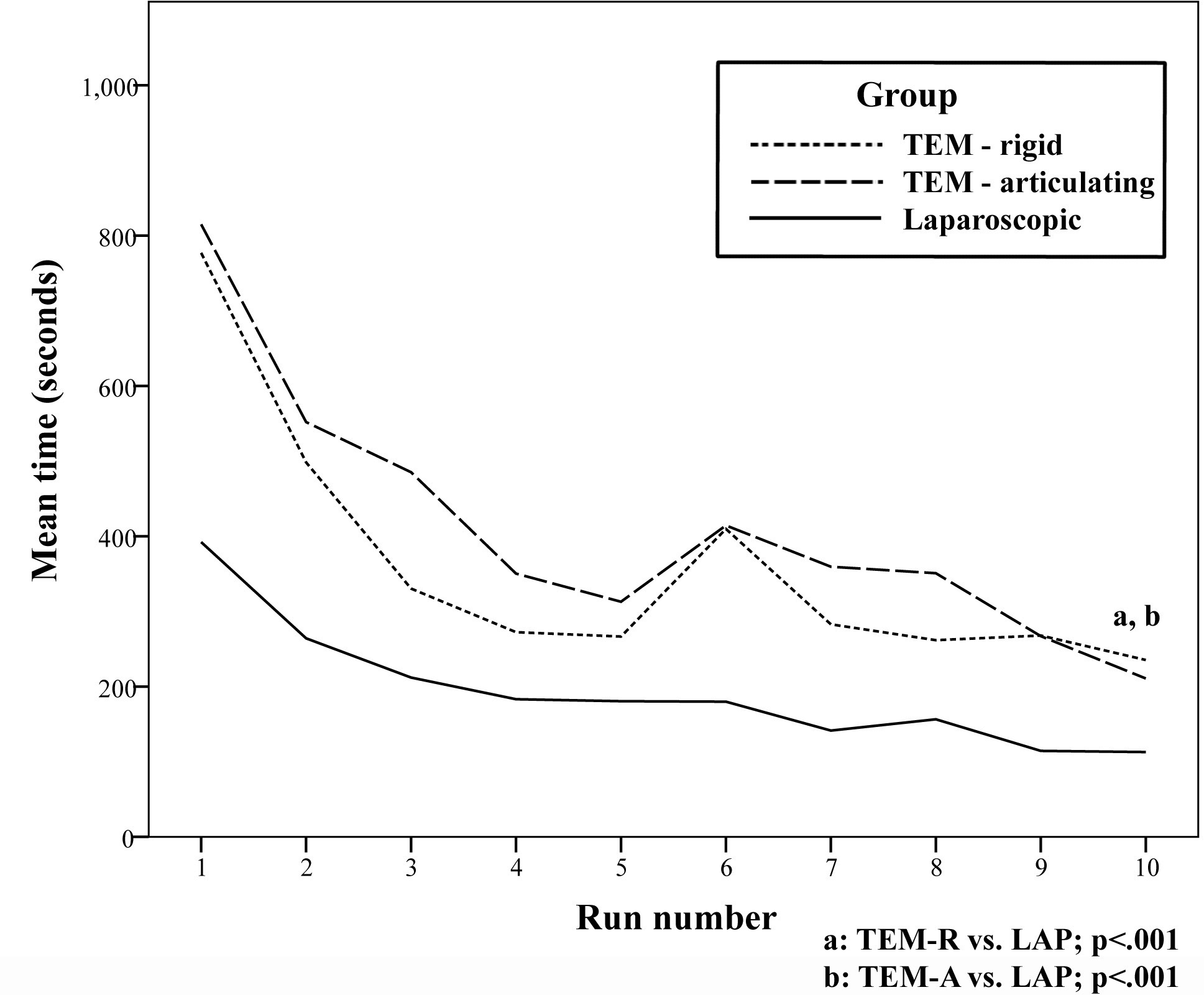
Background: The transanal endoscopic microsurgery (TEM) proctoscope is used to resect benign and early-stage malignant rectal tumors, and has received recent attention as a potential platform for transanal natural orifice surgery. No study has evaluated the effectiveness of different instrumentation types for TEM surgery. We tested whether learning curves for surgical novices using a TEM proctoscope would be improved with the use of scissors with shaft articulation. Additionally, we compared TEM and laparoscopic learning curves for the same task. Methods: Medical students were randomized into three study groups: laparoscopic (LAP), TEM rigid (TEM-R), and TEM articulating (TEM-A). All groups completed the Fundamentals of Laparoscopic Surgery (FLS) circle-cut task 10 times. The LAP group completed the task using an FLS box-trainer and a standard laparoscopic grasper and rigid laparoscopic scissors. The TEM-R group completed the task using the same instruments but through a TEM proctoscope within a custom TEM box-trainer. The TEM-A group completed the tasks using the same grasper but with scissors capable of shaft articulation up to 85 degrees. Outcomes were the standard FLS metrics of time and error (deviation as a percentage of total circle area). Instrument switches between hands and TEM position adjustments were also recorded. Overall group outcomes were compared using t-tests. Mixed models were used to compare changes over the 10 runs. Results: 33 subjects were randomized, 11 to each group. Overall mean task time was shorter for the LAP group than both the TEM-R and TEM-A groups (200 vs. 362 and 417 seconds; p<.001) (See Figure). Subjects in all three groups showed improvement in time over the 10 runs (coefficient estimates -33, -62, and -61; p<.001 for each group). The LAP group made fewer errors than the TEM-R group, but not the TEM-A group (7% vs. 10% vs. 8% circle area; p=.02 LAP vs. TEM-R). The LAP and TEM-A group made fewer errors over time (coefficient estimates -0.6 and -0.7; p<.01 for both), whereas the TEM-R group had a trend towards increased errors (coefficient estimate 0.4; p=0.1). The LAP group switched instruments between hands during fewer runs than both the TEM-R and TEM-A groups (9% vs. 30% vs. 24% of runs; p<.01). The TEM-A group adjusted the proctoscope position during fewer runs than the TEM-R group (36% vs. 54% of runs; p=.01). Conclusions: A LAP approach results in faster circle-cut task times than a TEM approach. While times were similar, TEM procedures using articulating scissors may result in fewer errors and less need to adjust proctoscope position as compared with rigid scissors. These results can be used to develop specific curricula and training strategies for TEM surgery. Back to Annual Meeting Posters
|
|||||||
© 2026 Society for Surgery of the Alimentary Tract. All Rights Reserved. Read the Privacy Policy.