|
Back to Annual Meeting Posters
Long Term Recurrence and Survival Rates in Gastrointestinal Stromal Tumours (GISTs) Treated by Minimally Invasive Surgery
Evangelos S. Photi*1, Helen Stubbings2, Laszlo Igali3, Edward Cheong3, Allan Clark1, Michael P. Lewis3
1Medicine, Norwich Medical School, Norwich, United Kingdom; 2Oncology Department, Norfolk and Norwich University Hospital, Norwich, United Kingdom; 3Oesophagogastric Cancer Centre, Norfolk and Norwich University Hospital, Norwich, United Kingdom
Introduction: Gastrointestinal Stromal Tumours (GISTs) are the most frequently occurring sarcoma of the GI tract. Current treatment usually involves resection of the tumour with consideration of adjuvant imatinib, depending on the risk of recurrence. Complete R0 resection is an important aspect of surgery though the surgical or pathological margin required is unclear. Laparoscopic resection is used increasingly for these tumours. We aimed to examine the risk of recurrence, both local and metastatic, after laparoscopic resection with a macroscopic 10mm margin. Risk of relapse can be estimated based on Miettinen and Lasota criteria and this can also be used to guide frequency of clinical follow-up and imaging.
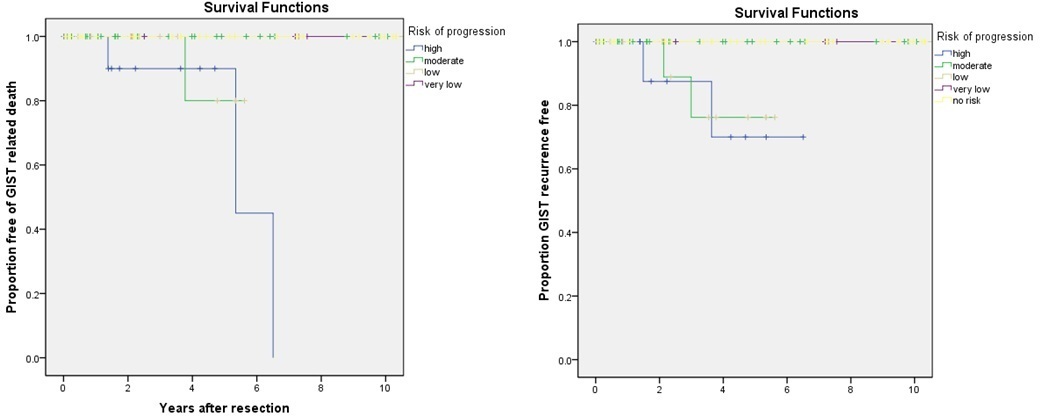
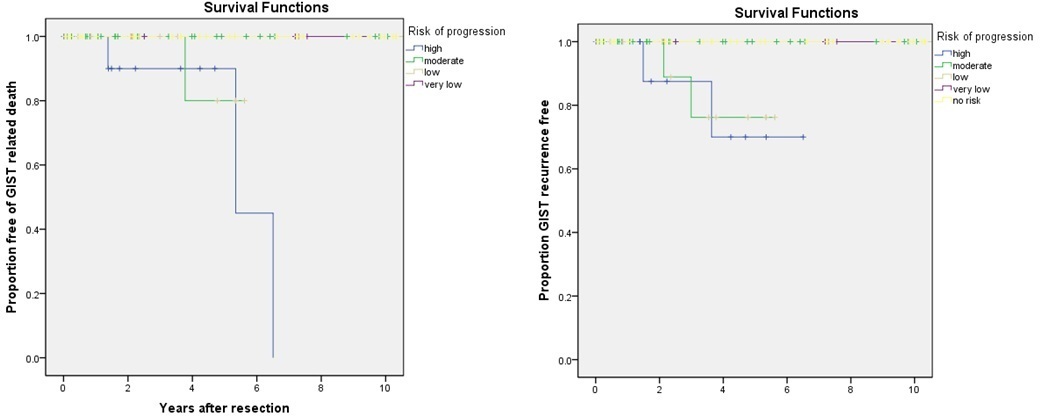
Methods: From the upper GI tumour database we identified primary non-metastatic GISTs of the upper GI tract treated by laparoscopic local resection. Cases were then graded for risk of progression based on histopathological findings using criteria such as tumour size, location within the GI tract and number of mitoses. This produced 5 risk groups: high, moderate, low, very low and no risk of progressive disease. Time to event was then calculated for each patient, the event being either death due to GIST, GIST recurrence (as evidenced on follow up CT abdomen/pelvis), or being recurrence free up to the end of the study.
Results: A total of 90 patients with primary upper gastrointestinal GISTs were identified from March 2000 to October 2012. The site of occurrence was gastric in 77 cases, small bowel in 11 cases, duodenal in 1 case and oesophageal in 1 case. Patients underwent surgical resection via a laparoscopic approach where possible with a standard local resection margin of 10mm (R0). Follow up was for a mean of 4.5 years.
Three patients in the high risk group who died of disease developed distant metastases (two patients with liver and one with peritoneal disease). Two other patients in the same group developed recurrence (one patient with liver and one with ileum/bladder metastases) but remain alive. One patient in the moderate risk group died of omental metastases. Two other patients developed liver metastases, one of whom died of thyroid cancer whilst on imatinib therapy and the other remains alive on imatinib therapy
The low and very low risk groups had a 10 year progression free survival of 100% with no incidences of GIST related death.
Conclusion: A 10mm surgical margin results in no local recurrence at up to 10 years. The low distant recurrence rate suggests that these tumours can safely be treated laparoscopically with an R0 resection using a surgical margin of 10mm. Distant recurrence is relatively low even in the high risk group for such tumours.
GIST related deaths and recurrences for each risk group.
| Risk Group | Number | Number of GIST related deaths | Number of GIST recurrences | | High | 11 | 3 | 2 | | Moderate | 11 | 1 | 2 | | Low | 31 | 0 | 0 | | Very low | 32 | 0 | 0 | | No risk | 5 | 0 | 0 |
Back to Annual Meeting Posters
|