|
Back to Annual Meeting Posters
Difference in Outcomes Between Right and Left Hepatectomy in Patients Undergoing Hepatic Resection
Mashaal Dhir*1, Lynette M. Smith1, George Dittrick2, Quan P. Ly1, Aaron R. Sasson1, Chandrakanth Are1
1University of Nebraska Medical Center, Omaha, NE; 2Surgery, Nebraska Methodist Hospital, Omaha, NE
Background: Several studies have documented the safety of liver resections. Although right hepatectomy is felt to be associated with higher mortality and morbidity, data on the difference in outcomes between right and left hepatectomy is scarce. The aim of the current study is to analyze the difference in outcomes between right and left hepatectomy in patients undergoing hepatic resection.
Methodology: All patients undergoing right (primary CPT code 47130) and left hepatectomy (primary CPT code 47125) were extracted from the National Surgical Quality Improvement Program (NSQIP) database (2005-2010). Benign and malignant diagnoses (ICD-9 155.0, 155.1, 155.2 and 197.7) were determined from the database. The data was analyzed to determine differences in outcomes between right and left hepatectomy by using the chi square test or Fisher's exact test as appropriate.
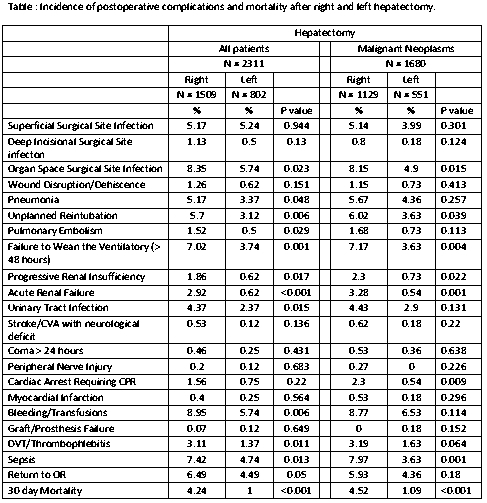
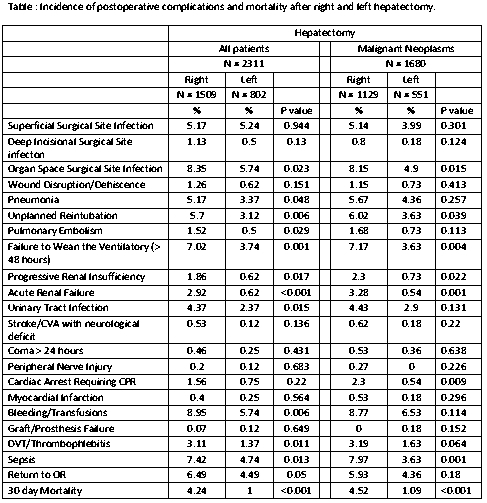
Results: A total of 2311 patients who underwent right or left hepatectomy were identified of whom 1680 patients were noted to have a malignant diagnosis. (Table 1) Patients that underwent right hepatectomy were noted to be have a higher mortality rate when compared to left hepatectomy (all patients: right vs left - 4.24% vs 1%, P < 0.001 and for patients with malignancy: right vs left - 4.52% vs 1.09%, P < 0.001). Right hepatectomy was also associated with significantly higher incidence of several other complications such as organ space infections, pneumonia, unplanned re-intubation, pulmonary embolism, failure to wean off the ventilator, renal insufficiency, urinary tract infection, blood transfusion, deep venous thrombosis and sepsis (P value < 0.05).
Conclusion: The results of our study demonstrate that mortality and morbidity after right hepatectomy remains significantly higher than left hepatectomy.
Back to Annual Meeting Posters
|