|
 |
Back to Annual Meeting Posters
Celiac Nodal Status As Determined by Laparoscopic Gastric Ischemic Preconditioning Is Prognostic in Locally-Advanced Esophageal Cancer and May Determine Necessity for Completion Esophagectomy
Sabha Ganai*2,1, Michael B. Ujiki1,2, Mark Talamonti1,2, John G. Linn1,2, Amy K. Yetasook1, Joann Carbray1, Marco Zahedi1, Ki Wan Kim1,2, John Howington1,2
1Surgery, NorthShore University HealthSystem, Evanston, IL; 2Surgery, The University of Chicago Medicine, Chicago, IL
Introduction: Laparoscopic gastric preconditioning has theoretical benefits of reducing conduit-related morbidity by allowing time for the stomach to adapt and/or demarcate to ischemic insults prior to staged esophagectomy and reconstruction. We hypothesized that focused pathological assessment of celiac lymph nodes during the conditioning interval could predict long-term outcomes after esophagectomy in patients with locally-advanced esophageal cancer.
Methods: A single-institutional retrospective review was conducted between 10/2008 and 11/2012, identifying 34 patients with locally-advanced (clinical Stage IIB/III) esophageal cancer who completed staged esophagectomy after laparoscopic preconditioning. Median follow-up was 9 months.
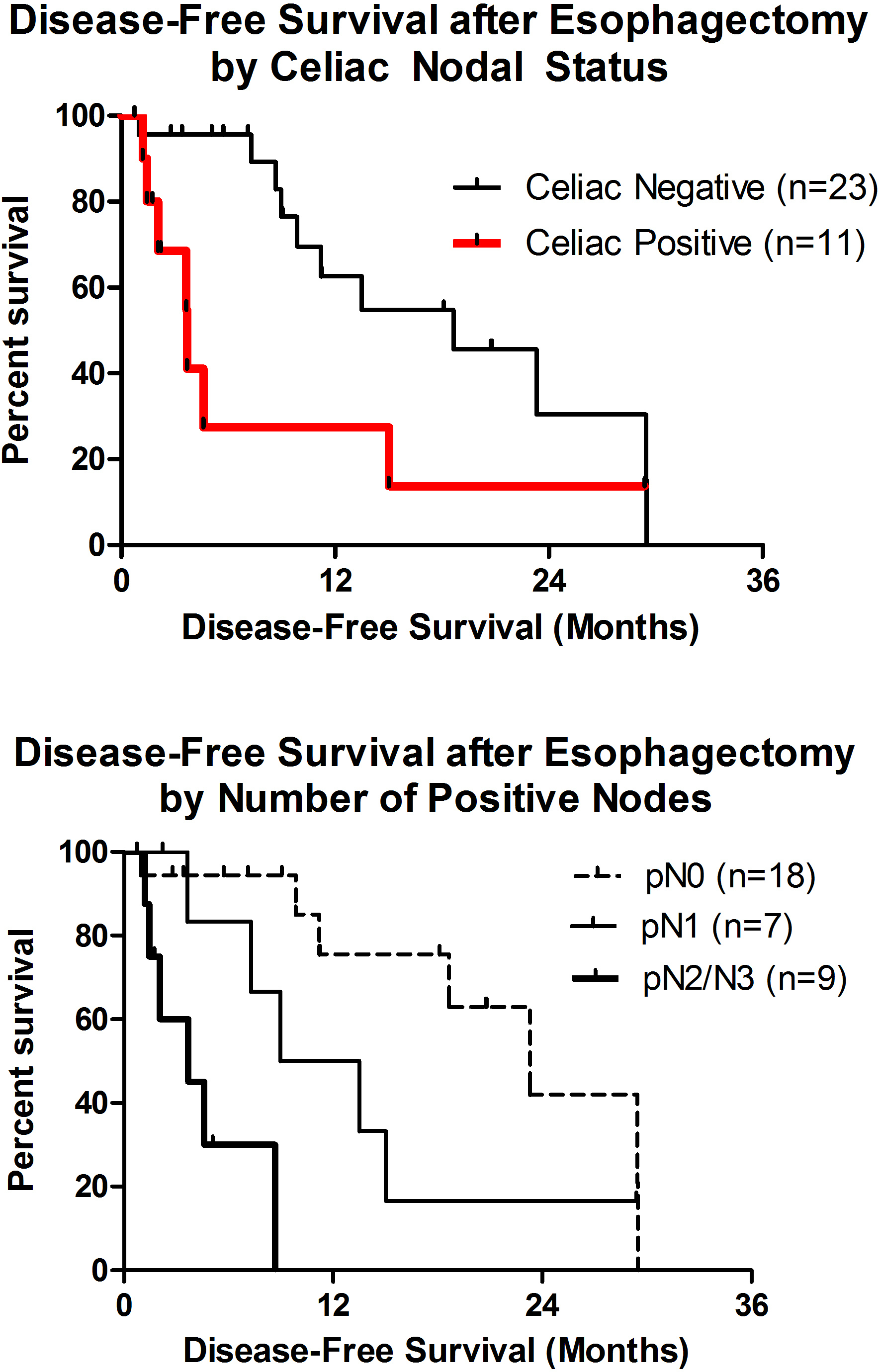
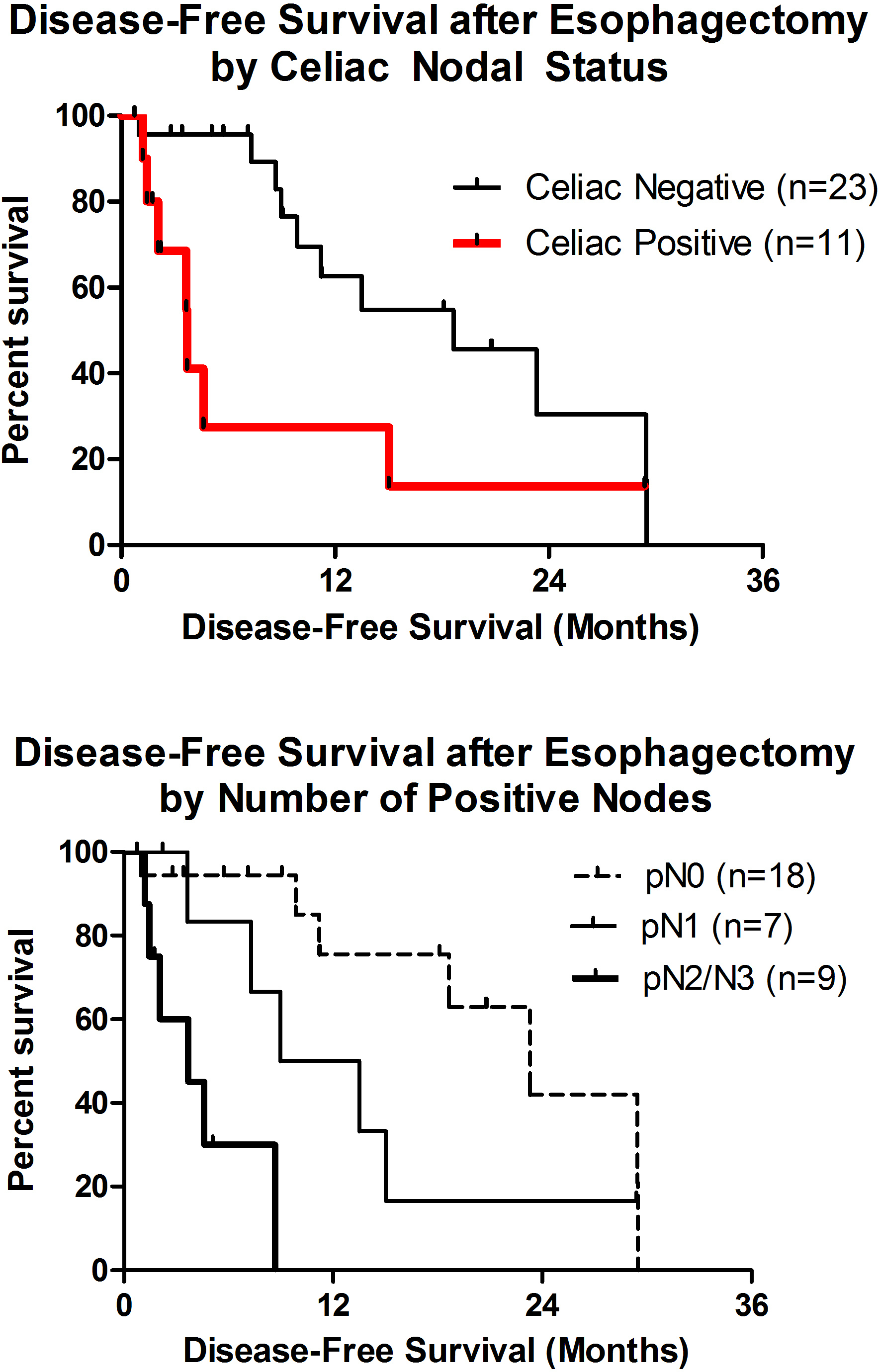
Results: Patients were 60±10 years old, 82% male, and had a BMI of 24±5 kg/m2. The median interval from preconditioning to esophagectomy was 7 days (interquartile range, IQR, 7-8). Preoperative staging was performed with EUS in 94% and PET in 100%, with 4 (12%) and 30 (88%) patients having clinical Stage IIB and III disease, respectively. Ninety-one percent of lesions were located in the distal esophagus, GE junction, and/or cardia. Histology comprised 30 (88%) adenocarcinomas, 3 (9%) squamous cell carcinomas, and 1 (3%) adenosquamous carcinoma. Ninety-seven percent of patients completed neoadjuvant therapy, with a pathologic complete response rate of 27%. All patients had microscopically-negative margins. The median number of lymph nodes resected was 20 (IQR 16-24), with a median of 5 (IQR 3-6) identified in the celiac nodal packet harvested during the preconditioning stage. Patients with positive celiac lymph nodes (32%) were more likely to have pN2/N3 disease (3 or greater positive nodes) than those with negative celiac nodes (64% versus 9%, p<0.01). Median disease-free survival by celiac lymph node status was 18.6 versus 3.7 months (HR 0.22, 95% CI 0.06-0.75, p<0.01). Median overall survival by pN status was 32.7 months for pN0, 12.2 months for pN1, and 5.6 months for pN2/N3 (p<0.001). On multivariate analysis controlling for histology, grade, pathological response to therapy, celiac nodal status, and pT status, only pN status remained an independent predictor of both disease-free (p<0.05) and overall survival (p<0.01).
Conclusions: While the AJCC 7th edition for staging of esophageal cancer has changed the emphasis from the location of regional lymph node metastasis to the number of positive nodes, our data suggest that esophagectomy may be avoided in patients with positive celiac nodes after neoadjuvant therapy for locally-advanced esophageal cancer. Laparoscopic preconditioning provides an opportunity to determine celiac nodal status prior to committing to esophagectomy.
Back to Annual Meeting Posters
|