|
Back to Annual Meeting Posters
Assessment of Postoperative Complications in Patients With IBD. a Single Academic Medical Center Experience
Samantha J. Quade*, Joshua Mourot, Anita Afzali, Mika N. Sinanan, Scott D. Lee, Jie Kate Hu, Christopher J. Park
General Surgery, University of Washington, Seattle, WA
Background: In Chrons Disease approximately 70% of all patients will ultimately require surgical intervention. Previous literature indicates that 30% of patients have postoperative complications. Pre operative nutrition with TPN has also been controversial.
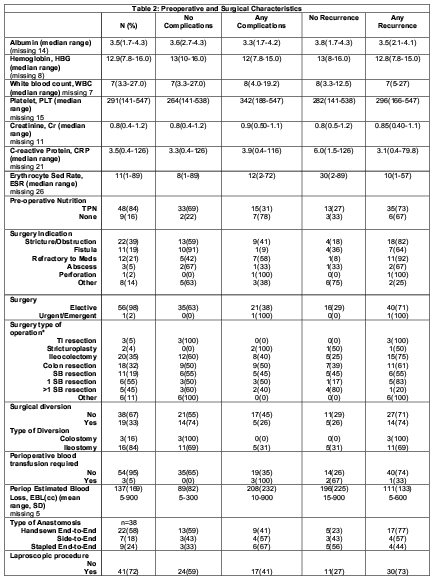
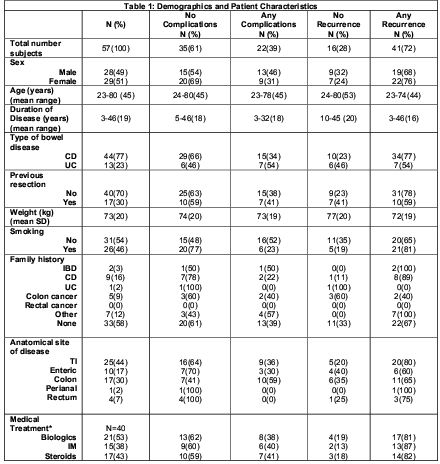
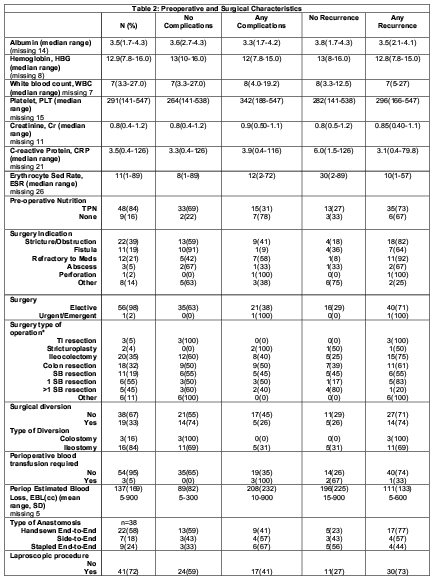
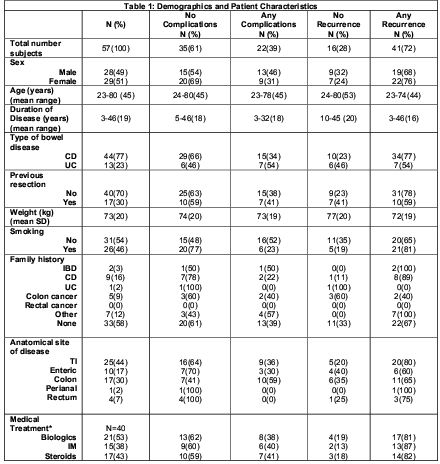
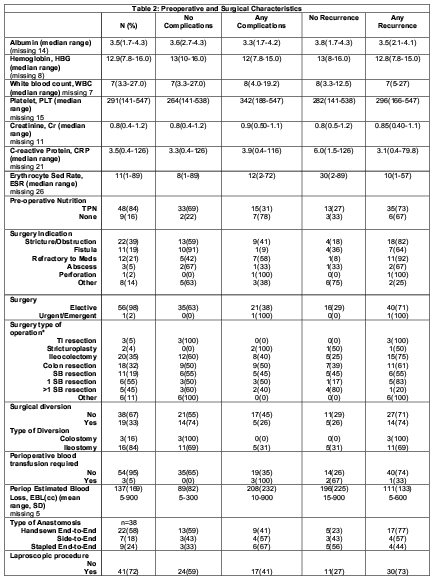
Our retrospective review demographics and patient characteristics were documented and both preoperative and surgical characteristics were identified to ascertain if the results from a single institution were congruent with the previous published literature.
Purpose: Assessment of post operative complications, pre operative predictive factors and need for reoperation and reinstitution of medical therapy in IBD.
Methods: Retrospective review of 57 patients charts who underwent surgical intervention for IBD. Patients undergoing surgical resection were included in the initial analysis.
Pre operative surgical characteristics, nutrition and surgical indication for intervention were analyzed.
The need for reoperation and reinstitution of medical therapy was based on patient symptoms and an endoscopic evaluation, which included a Rutgeerts score.
RESULTS: 57 patients [current analysis] 51% female, mean age 45 years, 30% of patients had undergone prior resection. 77% Chrons Disease.
Patient characteristics included 46% smoking, anatomical site of disease 44% TI disease, small bowel in 17% and colonic in 30%. Medical Therapy included Biologics in 53%, IM 38% and steroids in 43%.
Albumin mean 3.5g/dL [ postoperative early complications :mean 3.3 g/dL, no complications 3.6 g/dL].
Preoperative TPN 84% with an associated overall complication rate 31%.
Surgical Indication: Stricture/Obstruction 39%, Fistula 19%, Refractory to medications 21%, Abscess 5%, Perforation 2%.
Surgical Operation: Ileocolectomy 35%, TI resection 5%, stricturoplasty 4% and the remaining small bowel resection.
Type of anastomosis Hand Sewn end-to-end 58% patients [41% complication rate], side to end 18% [57% complication rate] and stapled end to end 24% [complication rate 67%].
Perioperative blood transfusion was required in 5% patients , 100% patients had complications.
Operative Blood Loss no complication 82cc and complication 232cc mean.
Perioperative length of stay mean 8 days [5.6 vs. 12.2 with post operative complication].
Overall Complication rate was 39%. Anastomotic leak rate 4%, Bowel obstruction 5%, prolonged ileus defined as > 5days 18%, Abscess formation 5%, Superficial wound infection 7% [no deep wound infections], UTI 5%, DVT 2%, PE 0%, Hernia 2%.
Reoperation required in 20% of patients.
CONCLUSIONS: Surgical Intervention for IBD can be associated with high morbidity and high rates of further medical and surgical intervention. Initial data analysis it appears that factors associated with a higher post operative complication rate are Albumin < 3.3, Perioperative Blood transfusion and stapled anastomosis.
Back to Annual Meeting Posters
|