|
Back to Annual Meeting Posters
Hepatic Metastasectomy Offers Improves Local Tumor Control Among Patients With Recurrent Colorectal Metastases
Victor M. Zaydfudim*1, Jeffrey S. Scow1, Grant D. Schmit2, Guido M. Sclabas1, Benzon Dy1, David M. Nagorney1
1Division of Gastroenterologic and General Surgery, Mayo Clinic, Rochester, MN; 2Department of Radiology, Mayo Clinic, Rochester, MN
Introduction:
Hepatic metastasectomy is an accepted treatment strategy for patients with colorectal metastases to the liver with demonstrated improvement in survival. Ablative strategies have been proposed for patients with recurrent liver metastases to avoid pitfalls of re-operative liver resection. The aim of this study was to evaluate the survival benefit of repeat metastasectomy and to compare hepatic resection to radiofrequency ablation (RFA) among patients with recurrent hepatic metastases.
Methods:
Patients continuously followed for primary colorectal malignancy, as well as, treatment of initial and recurrent colorectal metastases to the liver between 1992 and 2008 were included in this retrospective cohort study. Clinical variables were compared between patients treated with hepatic resection, hepatic ablation, or both treatment modalities for recurrent hepatic colorectal metastases. Independent radiologist, blinded to other covariates, categorized hepatic disease recurrence as local recurrence adjacent to the site of resection/ablation or new metastases.
Results:
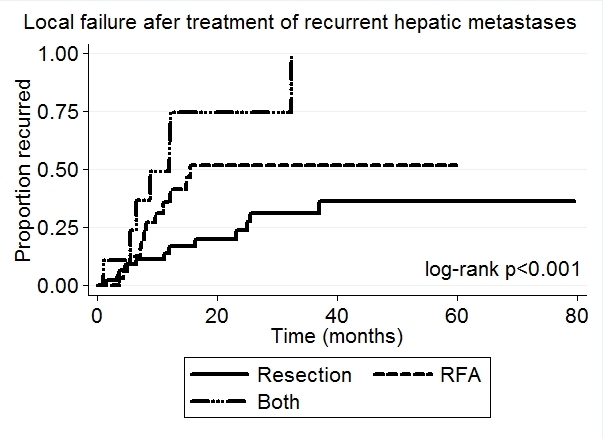
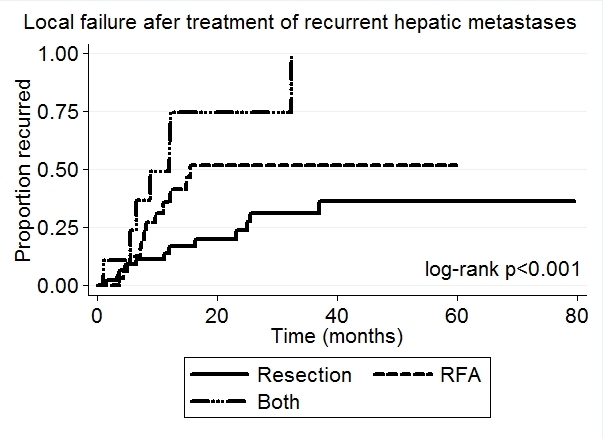
Ninety-three patients (median age 60 years (range 33-89), 57% male) were treated for recurrent hepatic metastases: 46 underwent recurrent hepatic resection, 38 underwent RFA, and 9 underwent both treatment modalities. Initial colorectal tumor stage, hepatic burden of initial liver metastases, anatomic resections of initial liver metastases, and disease free interval between primary resection and treatment of recurrent metastases did not differ between recurrent treatment groups (all p≥0.259). There was no difference in use of systemic therapy for treatment of initial and recurrent hepatic metastases (all p≥0.105). Only 19% of patients treated with RFA had more than one hepatic metastasis, compared to 33% of resected patients, and 100% of patients treated with both modalities (p<0.001). Among patients treated with hepatic metastasectomy, 15% underwent anatomic resection of ≥2 segments, while 85% underwent sub-segmental resections. 32 patients (34%) developed local re-recurrence at hepatic treatment site during a median of 12 months (range 1-142 months) follow-up with cross-sectional imaging after treatment of recurrent metastases. At 1- and 5- year follow-up, local recurrence rates were lowest among patients treated with hepatic metastasectomy compared to RFA and both treatment modalities: 17% vs. 41% vs. 75% at 1 year and 36% vs. 52% vs. 100% at 5 years, respectively (p<0.001, Figure). Overall survival did not differ between treatment groups (p=0.730)
Conclusions:
Metastasectomy offers improved local tumor control among patients with recurrent hepatic colorectal metastases and should remain the preferred treatment strategy for these patients. Majority of the patients with recurrent hepatic metastases are candidates for sub-segmental metastasectomy.
Back to Annual Meeting Posters
|