|
Back to Annual Meeting Posters
Prospective Study of Quality of Life After Laparoscopic Paraesophageal Hernia Repair With Bio-Prosthetic Mesh
Kashif a. Zuberi*1, Qingwen Kawaji2, Michael R. Marohn1, Miloslawa Stem1, Richard M. Fleming1, Michael Schweitzer1, Kimberley E. Steele1, Anne O. Lidor1
1Surgery, Johns Hopkins University School of Medicine, Baltimore, MD; 2Johns Hopkins Bloomberg School of Public Health, Baltimore, MD
Introduction:
Laparoscopic repair of paraesophageal hernia (PEH) with bio-prosthetic mesh (BP) has been shown to result in excellent relief of symptoms and improved quality of life (QOL) despite a relatively high recurrence rate. We evaluated our patient population to determine if change in quality of life is related to recurrence as well as specific risk factors that may increase the probability of recurrence after repair of PEH.
Methods and Procedures:
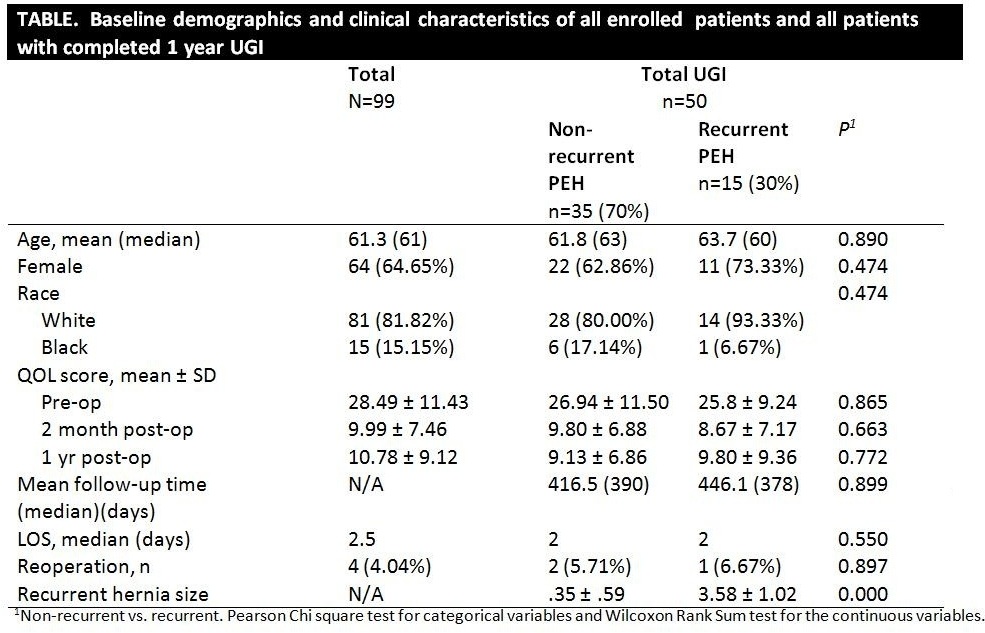
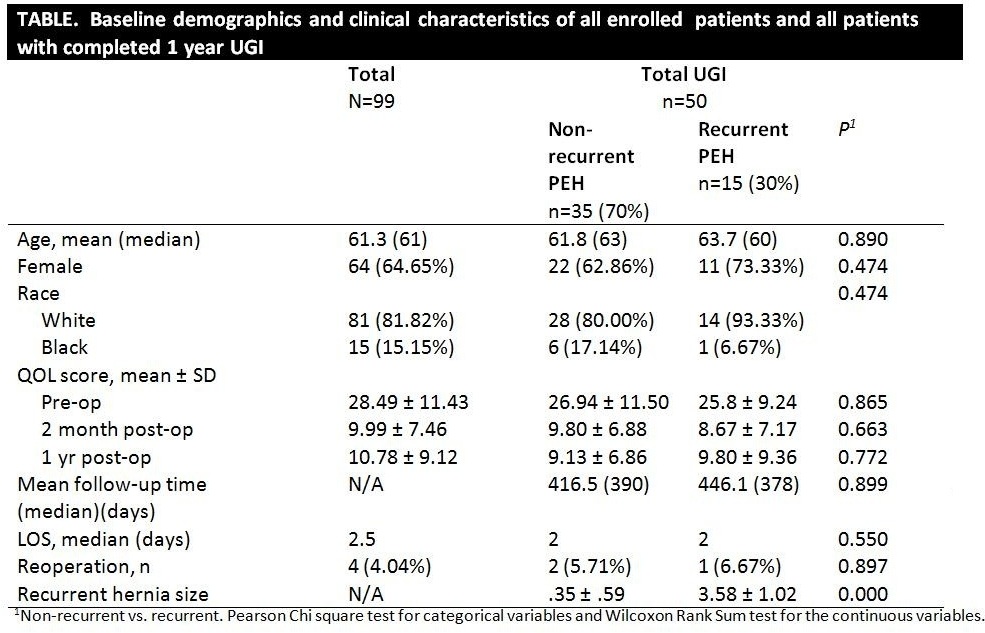
This is an analysis of data derived from an ongoing prospective study. From 4/2009 to 10/2012, we enrolled 99 patients who underwent elective laparoscopic PEH (type III) repair with BP (Veritas® collagen matrix, Synovis®, St. Paul MN) buttressed over a primary cruroplasty. All patients underwent Nissen fundoplication. A validated GERD-specific QOL tool was administered to patients before, and at 2 and 12 months post-operatively. UGI was performed at one year and recurrence was defined as a PEH greater than 2 cm. A single radiologist blinded to patient information read all studies. Demographic factors, comorbidities, and preoperative esophago-gastric testing were analyzed as possible indicators for recurrence. Approriate statistical analysis was used to compare variables. Univariate logistic regression was used to examine risk factors.
Results:
Overall 99 patients were analyzed. Median age was 61.3 years (range 24-89) with 64.65% women. Of 99 patients, 10 were not available for follow up and 50 reached their one year milestone and also underwent interval UGI. Four patients required reoperation, of which only one was for symptomatic recurrent PEH. The overall preoperative, 2 month, and 1 year QOL scores were 28.49, 9.99, and 10.78 respectively (p=0.00). Our recurrence rate was 30% (n=15) at a mean follow up of 425 days (range 234-802). The compared mean QOL scores between the preoperative, two month, and one year follow-up were all statistically significant. The symptoms of early satiety and dysphagia did not improve in the patients in whom a recurrence was detected, otherwise there was significant improvement in all other individual symptoms assessed in the QOL tool. There was no association between diabetes, smoking history, the use of gastropexy, or previous abdominal surgery and PEH recurrence. Preoperative testing with manometry and gastric emptying studies were statistically unable to identify patients at risk of recurrence.
Conclusion:
Our analysis of difference in symptom scores after laparoscopic PEH repair suggests that significant worsening occurs with radiologically recurrent hernias > 2cm with respect to early satiety and dysphagia. We were unable to demonstrate at one year follow up if any specific risk factors increase the incidence of recurrence. Overall, patients with recurrent PEHs continue to experience excellent QOL and rarely require re-operation.
Back to Annual Meeting Posters
|