|
Back to Annual Meeting Posters
The Clinical Spectrum of Esophagogastric Junction Outflow Obstruction Identified via High Resolution Manometry
Poochong Timratana*, Michal J. Lada, Dylan R. Nieman, Michelle S. Han, Christian G. Peyre, Carolyn E. Jones, Thomas J. Watson, Jeffrey H. Peters
Department of Surgery, University of Rochester Medical Center, Rochester, NY
Introduction: The identification of esophagogastric junction (EGJ) outflow obstruction via high resolution manometry (HRM) is increasingly common and of unclear clinical significance. The objective of this study was to review the HRM characteristics of EGJ outflow obstruction and to assess how this diagnosis translates into clinical practice.
Methods: A retrospective review was conducted of 1105 symptomatic patients who underwent HRM between 9/09 and 8/12. EGJ outflow obstruction was defined as an elevated 4 second lower esophageal sphincter integrated relaxation pressure (IRP). Patients with elevated IRP were divided into 3 groups: achalasia, mechanical obstruction (large hiatal hernia, postoperative and neoplasia) and functional obstruction (no obvious underlying cause). Clinical and demographic data, presenting symptoms, upper endoscopic findings, treatment and post-treatment outcomes were compared among the groups.
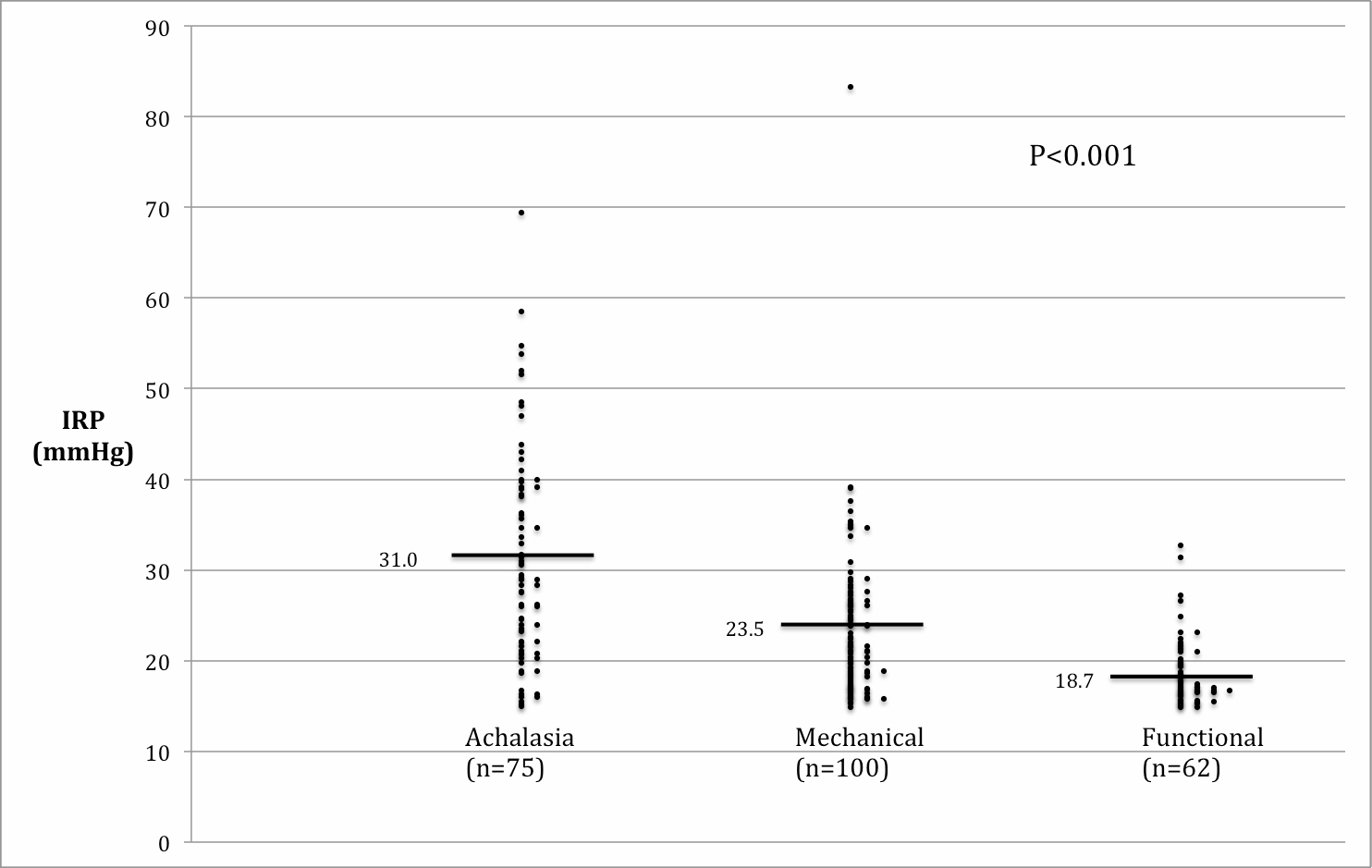
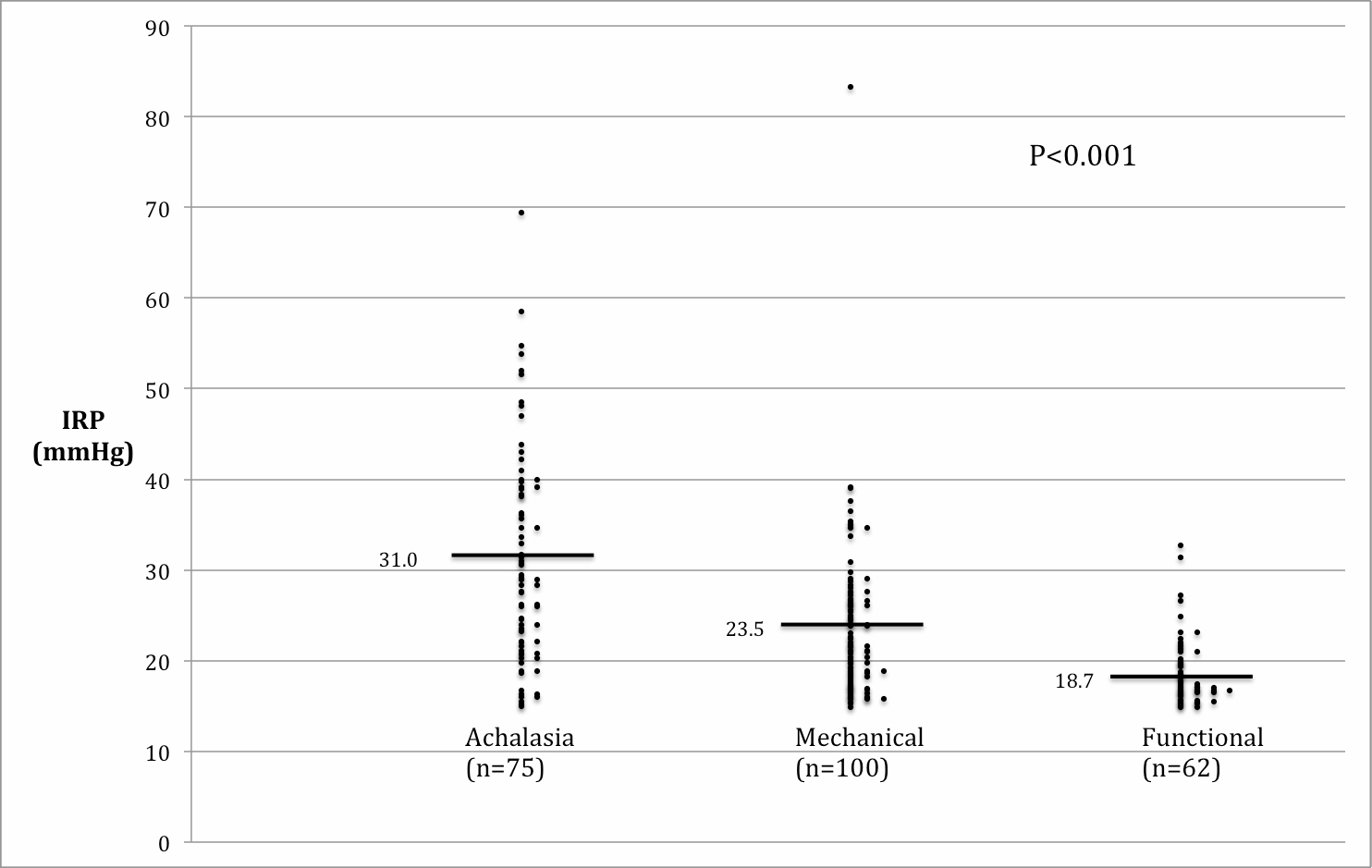
Results: Of the 1105 patients studied, 237 (21%) had an elevated IRP. Sixty four percent were female with a mean age of 56.8±15.4 years. Mechanical causes of obstruction were most common (100/237, 42%) including postoperative in 50, large hiatal hernia in 48 and esophageal cancer in 2. Achalasia was present in 75 patients (32%). The remaining 62 (26%) had an elevated IRP without evidence of mechanical obstruction. Dysphagia was the primary presenting symptom in 85% of patients in the achalasia group, 31% of the mechanical group and 13% of the functional group (p<0.009). Interestingly, upper respiratory symptoms were significantly more common in patients with functional outflow obstruction (26% vs. 1% achalasia and 4% mechanical, p<0.001). The mean IRP also varied amongst the clinical groups, highest in achalasia 31.0±11.7mmHg, intermediate in mechanical obstruction (23.5 ±8.6 mmHg) and lowest in the functional group (18.7±3.8 mmHg) p<0.001. A similar pattern was seen in the mean intra-bolus pressures 28.6±15.0 mmHg, 20.1±7.4 mmHg and 14.9±4.0 mmHg, respectively. Nearly 40% (22/57) of the patents with functional outflow obstruction parameters were pH positive suggesting GE barrier failure despite the manometric findings. Fundoplication was performed in 9 of these 22 patients (41%) with good response. Five of the remaining functional patients underwent treatment; myotomy in one and Botox in 4.
Conclusions: The predominant etiologies of EGJ outflow obstruction are mechanical obstruction and achalasia. Mechanical causes should be excluded before functional outflow obstruction is diagnosed and treated. HRM parameters of functional outflow obstruction may be present in a subset of patients with pH positive GERD. The ideal management of patients with symptomatic functional obstruction remains unclear.
Back to Annual Meeting Posters
|