|
Back to Annual Meeting Posters
Outcomes of Esophagectomy for Esophageal Achalasia in the United States
Daniela Molena*, Miloslawa Stem, Anne O. Lidor
Surgery, Johns Hopkins University School of Medicine, Baltimore, MD
Background: While the outcomes after Heller myotomy have been extensively reported, little is known about patients with esophageal achalasia who are treated with esophagectomy.
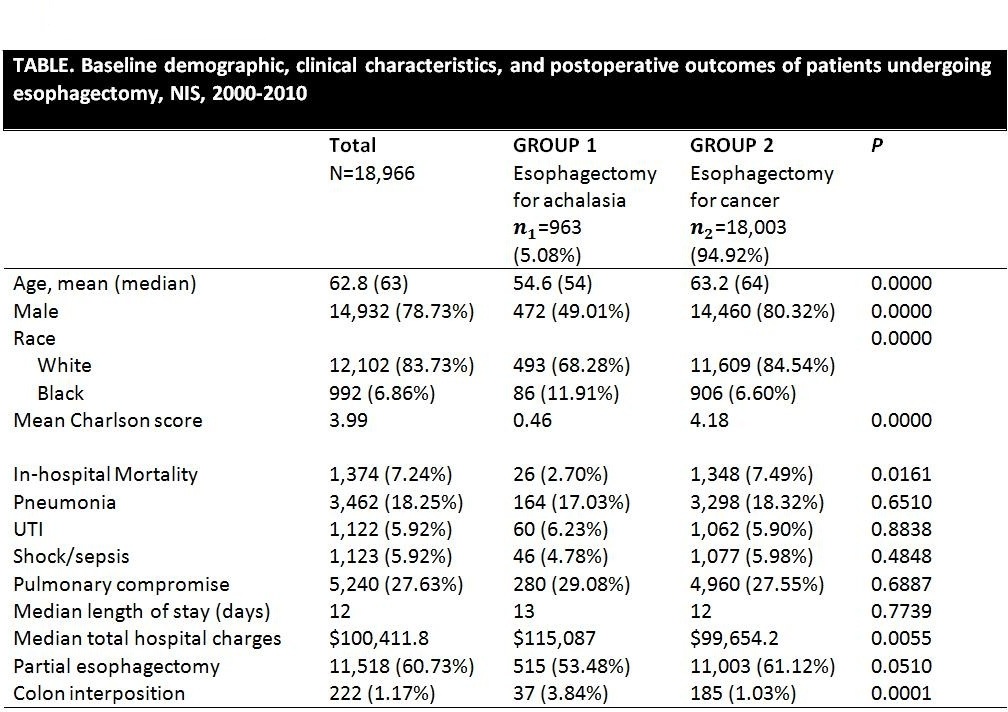
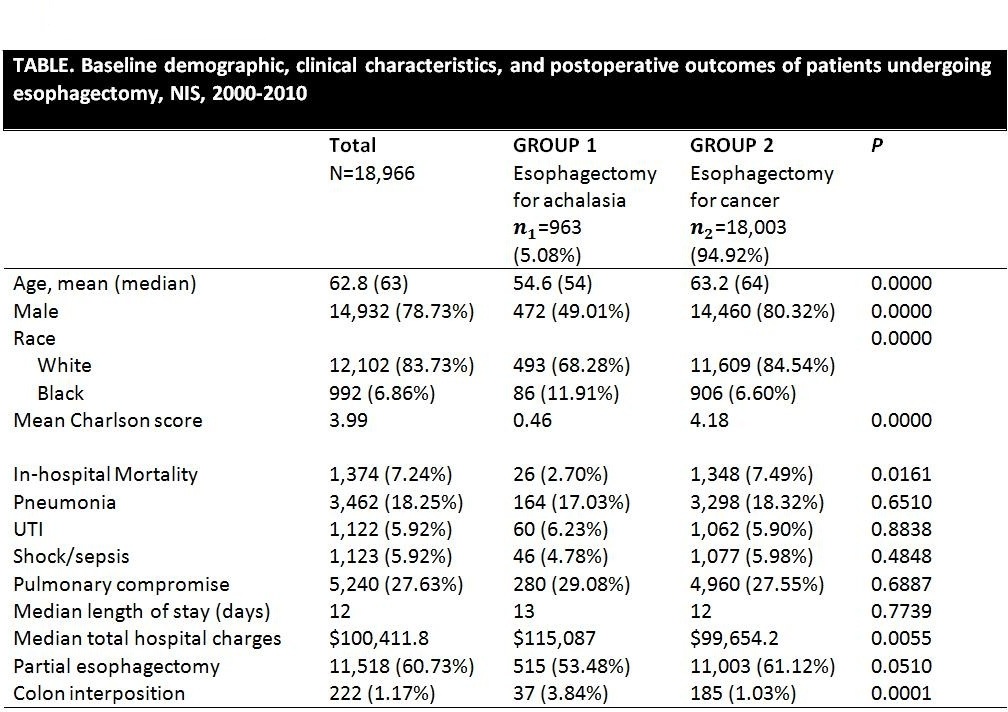
Methods: This was a retrospective analysis using the Nationwide Inpatient Sample over an 11-year period (2000-2010). Patients admitted with a primary diagnosis of achalasia who underwent esophagectomy (Group 1) were compared to patients with esophageal cancer who underwent esophagectomy (Group 2) during the same time period. Primary outcome was in-hospital mortality. Secondary outcomes included length of stay (LOS), post-operative complications and total hospital charges. A propensity-matched analysis was conducted comparing these same outcomes between Group 1 and well-matched controls in Group 2 during the same era.
Results: Among 43,668 patients admitted with a primary diagnosis of achalasia, 963 (2.2%) underwent esophagectomy. The overall in-hospital mortality in Group 1 was 2.7%. The most common post-operative complications in this group were pneumonia (17%) and pulmonary compromise (29%). During the same time period, 18,003 patients with esophageal cancer underwent esophagectomy. Patients in Group 1 were younger, healthier, and had a lower mortality when compared to Group 2. Post operative LOS and complications were similar in both groups, although hospital charges were significantly higher in Group 1. (Table 1). The most common surgical procedure was a partial esophagectomy in both groups. The number of colon interpositions was higher in Group 1 (1% versus 4%, p=0.0001). The propensity matched analysis showed a trend toward a higher mortality in Group 2 (7.8% versus 2.9%, p=0.08). Among patients who died in both groups the most common associated diagnosis codes were respiratory complications and sepsis. Older male patients had the highest mortality among patients with achalasia.
Conclusion: This is the largest study to date examining outcomes after esophagectomy in patients with achalasia. In these patients, unadjusted mortality is statistically lower than in patients with esophageal cancer, while operative morbidity appears comparable. In a propensity matched analysis, there remains a trend toward lower mortality in Group 1. Based on these data, esophagectomy can be considered a safe option, and surgeons should not be hindered by a perceived notion of prohibitive operative risk in this patient population.
Back to Annual Meeting Posters
|