|
Back to Annual Meeting Posters
Surgical Stricturoplasty in the Treatment of Pouch Strictures
Xian-Rui Wu*1, Saurabh Mukewar2, Pokala R. Kiran1, Feza H. Remzi1, Bo Shen2
1Departments of Colorectal Surgery, Cleveland Clinic, Cleveland, OH; 2Department of Gastroenterology/Hepatology, Cleveland Clinic, Cleveland, OH
Objective: To evaluate the efficacy of stricturoplasty in the treatment of pouch strictures in comparison with endoscopic balloon dilation.
Summary Background Data: There was only one case report on surgical stricturosplasty in treating pouch strictures.
Methods: Consecutive inflammatory bowel disease (IBD) patients with ileal pouch strictures seen in our Pouchitis Clinic from 2002-2012 were studied. Efficacy and safety were evaluated with both univariate and multivariate analysis.
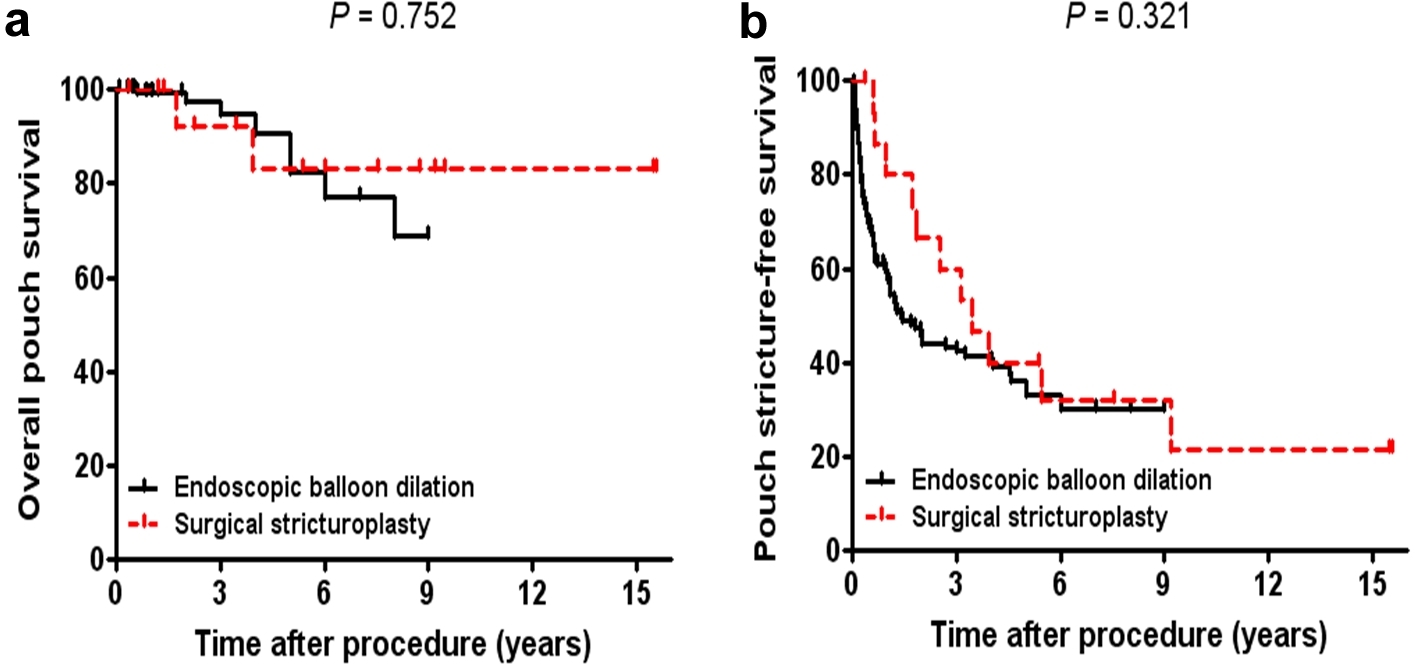
Results: A total of 167 patients met the inclusion criteria, including 16 (9.6%) who had surgical stricturoplasty and 151 (90.4%) had at least one endoscopic stricture dilation therapy. Ninety-four patients (56.3%) were male, with a mean age at the diagnosis of pouch strictures of 41.6±13.2 years. Fifty-one patients (30.5%) had multiple pouch strictures, and pouch inlet strictures occurred in 100 (59.9%). The mean length of pouch strictures was 1.2±0.6 cm. No difference was identified between the stricturoplasty and dilation groups in clinicopathological variables, except for degree of strictures (P=0.019). After a mean follow-up of 4.1±2.6 years, pouch stricture recurred in 92 patients (55.1%) and 21 (12.6 %) developed pouch failure. The time interval between the procedure and pouch stricture recurrence or pouch failure was longer in the stricturoplasty group than in the dilation group (P<0.001). Although patients in the two groups had a similar overall pouch survival (5-year overall-pouch-survival: 83.1% vs. 82.0%), patients treated with stricturoplasty seemed to bear a better pouch stricture-free survival than those with endoscopic balloon dilation (5-year pouch-stricture-free-survival: 39.8% vs. 33.1%). There was no difference in complication rates between the two groups.
Conclusions: Patients with pouch strictures had a similar overall pouch survival after being treated with stricturoplasty and endoscopic balloon dilation. Surgical stricturoplasty tended to have a better stricture-free survival benefit.
Table. Multivariate Analysis of the Risk Factors Associated with Overall Pouch Survival and Pouch Stricture-free Survival.
| Characteristic | Hazard ratio | 95% CI | P Value | | Overall Pouch Survival | | Postop use of biologics (yes vs no) | 6.249 | 2.296-17.012 | <0.001 | | Degree of stricture (3 vs 1 or 2) | 4.125 | 1.707-9.970 | 0.002 | | Post-IPAA complications (yes vs no) | 5.528 | 2.038-14.995 | 0.001 | | Treatment modality (stricturoplasty vs endoscopic balloon dilation) | 0.974 | 0.205-4.632 | 0.973 | | Pouch Stricture-free Survival | | Number of stricture (≥2 vs 1) | 4.827 | 3.167-7.356 | <0.001 | | Degree of stricture (3 vs 1 or 2) | 2.005 | 1.239-3.245 | 0.005 | | Treatment modality (stricturoplasty vs endoscopic balloon dilation) | 0.548 | 0.279-1.075 | 0.080 |
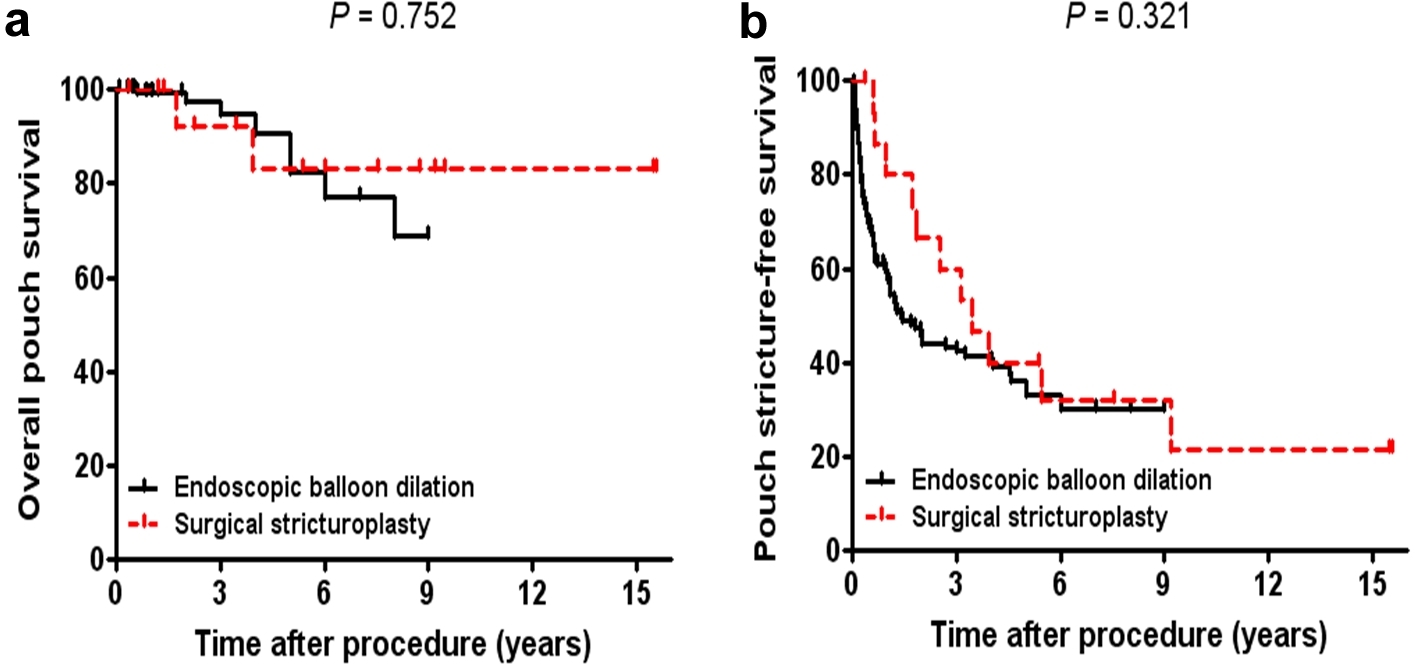
Table. Multivariate Analysis of the Risk Factors Associated with Overall Pouch Survival and Pouch Stricture-free Survival.
Back to Annual Meeting Posters
|