|
 |
Back to Annual Meeting Program
Failure to Receive Adjuvant Therapy Following Resection for Pancreatic Cancer: Patterns and Implications
Russell S. Lewis*1, Jeffrey a. Drebin1, Mark P. Callery2, Douglas L. Fraker1, Tara S. Kent2, Jenna Gates1, Charles M. Vollmer1
1Surgery, The University of Pennsylvania School of Medicine, Philadelphia, PA; 2Surgery, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
<p>Introduction: Although adjuvant therapy optimizes the prognosis for resected pancreatic ductal adenocarcinoma (PDAC), literature indicates that this approach is not applied in up to half of patients. This has prompted some to advocate preoperative adjuvant therapy to ensure receipt of all elements of multidisciplinary oncologic care. We sought to identify the frequency, reasons, and predictors of unutilized post-operative adjuvant therapy in a multidisciplinary, specialty setting.
<p>
Methods: A database containing PDAC resections performed at two institutions over a decade (2001-2011) was studied. Eligible patients who did not undergo adjuvant therapy were identified and categorized based on the rationale for not receiving treatment. Demographics, perioperative features, tumor characteristics, and surgical risk scores (ASA, POSSUM, Charlson, SOAR) were analyzed by univariate analysis and multivariate regression to assess factors associated with these untreated patients, focusing further on a subset that displayed poor clinical outcomes.
<p>
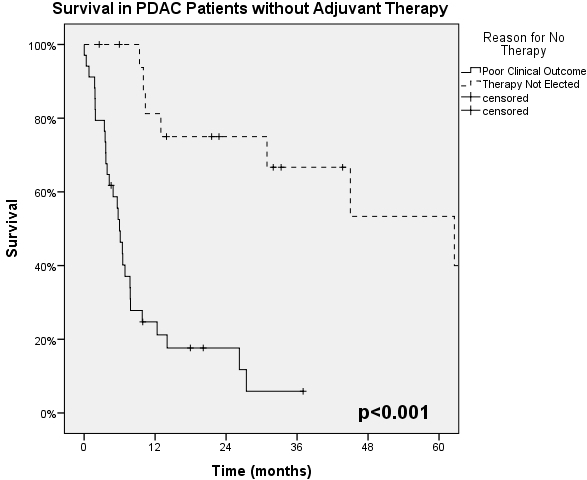
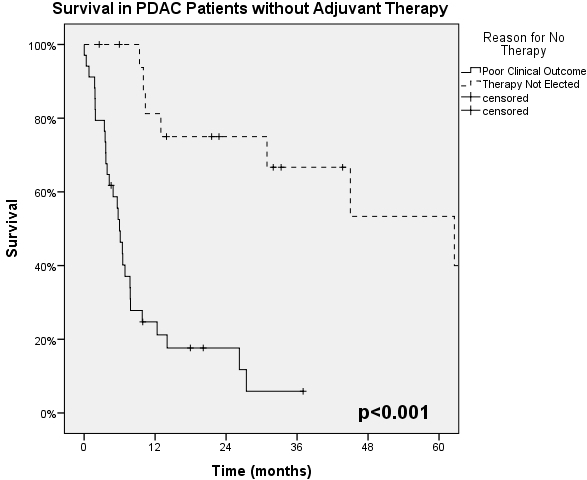
Results: Of 412 resected PDAC patients 336 (82%) received some form of postoperative treatment, while only 52 (including 90d mortalities, N=7) did not. Treated patients had median, 1- & 5-year survivals of 23.5 mo, 80% & 25%, compared to 9.4 mo, 44% & 22% in the Untreated group (p<.001). 24 patients whose treatment status is unknown exhibited equivalent survival to the treated cohort (19.3 mo, 78% & 17%; p=.296). Characteristics of the Untreated cohort by multivariate analysis were advanced age, complications, lack of jaundice, and IPMN. Early tumor progression was identified in seven of these patients. Four principal reasons for unutilized therapy were identified (Table). These segregated into two disparate groups - Poor Clinical Outcomes (2/3rds) and Therapy Not Elected (1/3rd), which demonstrated a marked median survival difference (6.0 mo vs. 62.6 mo respectively; p<0.001, Graph). The Therapy Not Elected group was characterized by favorable tumor biology. The Poor Clinical Outcome group contained two-thirds of all Major complications (Clavien 3b-5) in this entire series. When scrutinized further by multivariate analysis, the only preoperative factors associated with this group were older age and COPD, and this cohort could not be discriminated by preoperative risk scoring systems.
<p>
Conclusions: This series demonstrates that the vast majority of PDAC patients can receive post-operative adjuvant therapy following surgical resection. There are various reasons for non-utilization, not all of which represent inadequate care. The ability to employ adjuvant therapy is predicated on optimal surgical outcomes. Pre-operative prediction of the minority of patients with poor outcomes that prevent adjuvant treatment, using current risk assessment models, remains elusive.
Patients Who Did Not Receive Adjuvant Therapy after Pancreatic Resection - Categorized By Reasons
| Frequency | Survival | | n | % | Median (mo) | 1yr | 3yr | 5yr | | <P ALIGN="left">Poor Clinical Outcome | 34 | 65.4 | 6.0 | 24% | 5% | n/a | | <P ALIGN="left">1. Early Death (90d) | 7 | 13.5 | 1.8 | 0% | 0% | 0% | | <P ALIGN="left">2. Diminished Functional Capacity (Complications/Early Recurrence) | 27 | 51.9 | 6.9 | 31% | 7% | n/a | | <P ALIGN="left">Therapy Not Elected | 18 | 34.6 | 62.6 | 82% | 66% | 54% | | <P ALIGN="left">3. Declined Against Medical Advice - Patient's Choice | 8 | 15.4 | 10.4 | 57% | 0% | 0% | | <P ALIGN="left">4. Deemed Unnecessary - Physician's Choice | 10 | 19.2 | Not Reached | 100% | 100% | 82% | | <P ALIGN="left">Total | 52 | 100.0 | 9.4 | 44% | 27% | 22% |
Back to Annual Meeting Program
|