Back to 2025 Posters
TRANSORAL OUTLET REDUCTION FOR TREATMENT OF REFRACTORY BILE ACID ESOPHAGITIS AFTER ROUX-EN-Y GASTRIC BYPASS AND BRAUN ENTEROENTEROSTOMY
Derek J. Scholes
*1,2, Vanessa F. Eller
1,2, Farah Husain
1, Mackenzie Landin
1, Kevin Liu
11Internal Medicine, Banner - University Medical Center Phoenix, Phoenix, AZ; 2The University of Arizona College of Medicine Phoenix, Phoenix, AZ
Bile acid reflux is a recognized complication following Roux-en-Y gastric bypass (RYGB) and occurs due to anatomical changes that facilitate bile pooling in the gastric pouch, which can result in potentially chronic and debilitating abdominal pain. Initial management involves treatment with bile acid sequestrants such as ursodeoxycholic acid and PPI therapy. We present a case of a patient who developed medically refractory bile acid reflux after RYGB revision with Braun enteroenterostomy who was successfully treated by TORe with resolution of her esophagitis.
A 51-year-old female with prior RYGB complicated by marginal ulcer was initially evaluated by bariatric surgery for persistent abdominal pain and nausea. She underwent diagnostic laparoscopy and was found to have significant adhesions along the roux and biliopancreatic limb that required adhesiolysis. Two days postoperatively, she developed symptoms consistent with a small bowel obstruction and underwent repeat laparoscopy. This was notable for a significantly dilated biliopancreatic limb without an overt source of obstruction. A Braun enteroenterostomy was then performed upstream of the jejunojejunal anastomosis to decompress the dilated biliopancreatic limb.
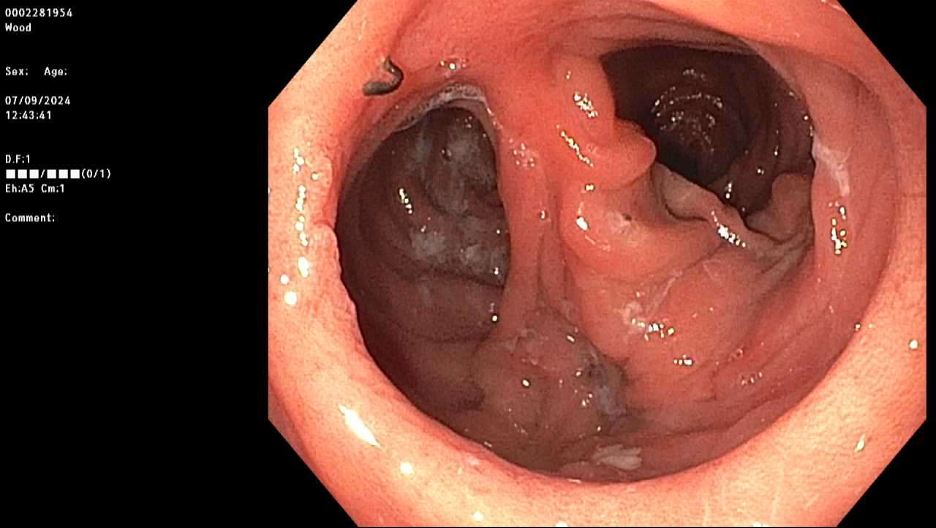
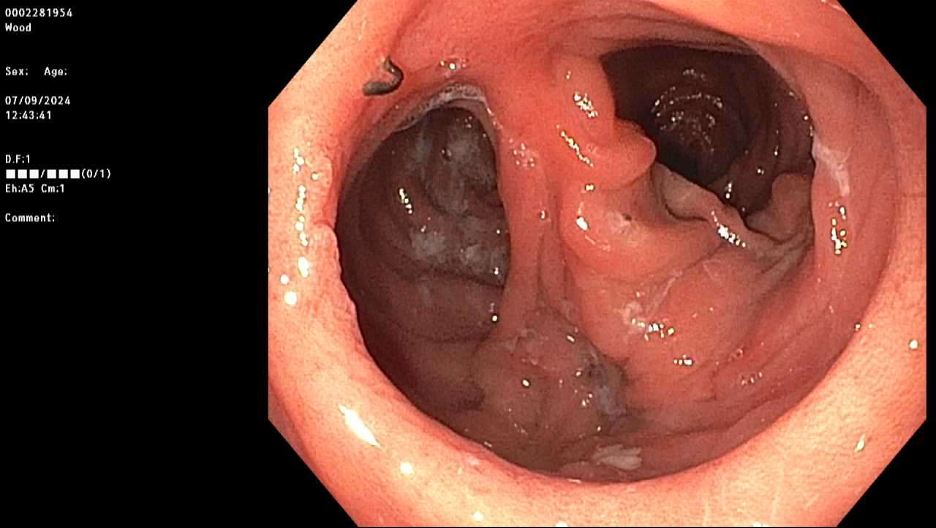
After surgery, the patient developed severe and intractable reflux. She underwent an EGD and was found to have LA grade B erosive esophagitis, which was not seen on the pre-operative endoscopy. Her gastrojejunal outlet was noted to be dilated at 30 mm. It was felt the bile acid reflux was likely due to the Braun enteroenterostomy and exacerbated by the dilated GJ. She was initially trialed on PPI and bile acid sequestrants including cholestyramine and colestipol with mild relief of her symptoms. She had also noted weight recurrence in the past several years and loss of a sensation of restriction with eating.
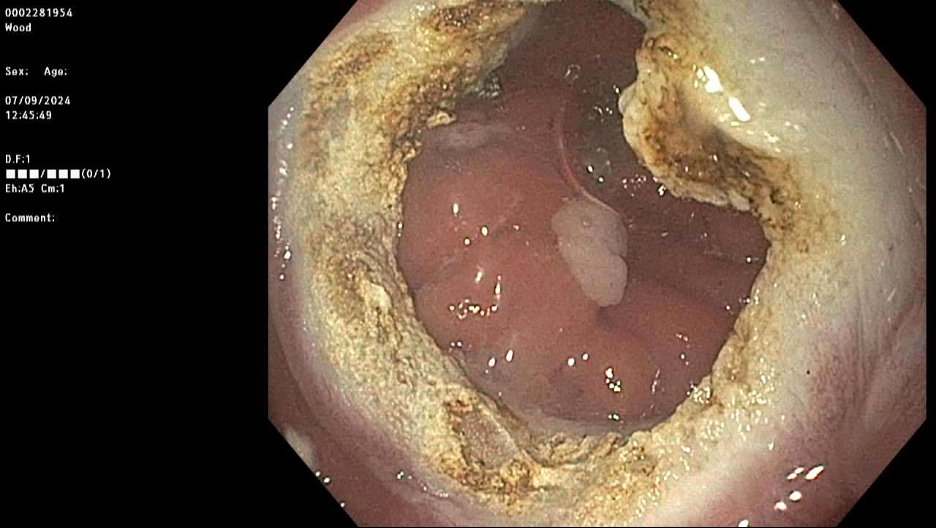
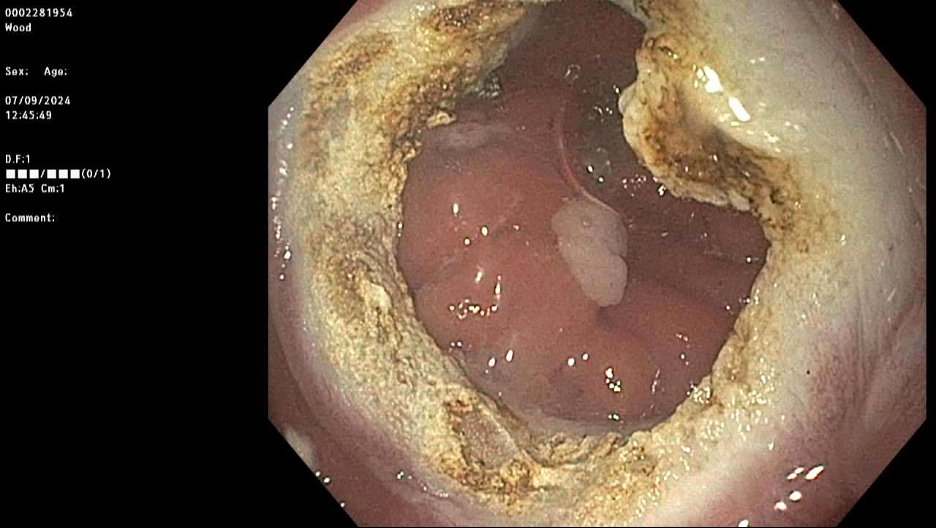
The decision was made to proceed with TORe for both treatment of weight recurrence and bile acid reflux. She underwent EGD with TORe with purse-string suturing and closure of the outlet to 8 mm. At her three-month follow-up, she reported a 25-pound weight loss and complete resolution of reflux symptoms. She was able to discontinue PPI and bile acid sequestrants and remained asymptomatic.
This case highlights TORe as an unusual but successful therapeutic modality for treatment of refractory bile acid reflux in a patient with history of RYGB, Braun enteroenterostomy and dilated gastrojejunal outlet. TORe has gained increasing recognition for treatment of weight recurrence in patients with dilated GJ outlet after RYGB. To our knowledge, this is the first case report of the use of TORe for treatment of refractory bile acid reflux in a patient with RYGB and dilated GJ outlet.
Back to 2025 Posters