Back to 2025 Posters
SURGICAL OUTCOMES IN ACHALASIA CARDIA: DOES LOWER ESOPHAGEAL SPHINCTER PRESSURE MATTER?
Utpal Anand
*, Bijit Saha
Surgical Gastroenterology, All India Institute of Medical Sciences, Patna, Patna, Bihar, India
Background: Achalasia cardia is diagnosed using high-resolution manometry (HRM), characterized by an integrated relaxation pressure (IRP) exceeding 15 mm Hg. Laparoscopic Heller Myotomy (LHM) is the established treatment for reducing lower esophageal sphincter pressure (LESP). However, less than half of achalasia patients exhibit elevated LESP. This study primarily investigates the impact of LESP on the outcomes of surgical treatment for achalasia.
Patients and Methods: Between 2019 and 2023, 52 patients underwent laparoscopic Heller myotomy with anterior Dor fundoplication. Preoperative evaluations included high-resolution esophageal manometry (HRM), video esophagogram, and upper gastrointestinal endoscopy. Patients were stratified into two groups based on HRM results: normal lower esophageal sphincter pressure (LESP ? 35 mm Hg, n = 30) and high LESP (LESP > 35 mm Hg, n = 22). Symptoms were assessed preoperatively and at a median follow-up of 24 months using standardized scoring systems, including the Eckardt score (ES; 0-12) for dysphagia, regurgitation, weight loss, and chest pain, and the Achalasia Symptom Questionnaire (ASQ; 0-33) for quality of life. Treatment failure was defined as an ES ? 4 or an ASQ score ? 16.
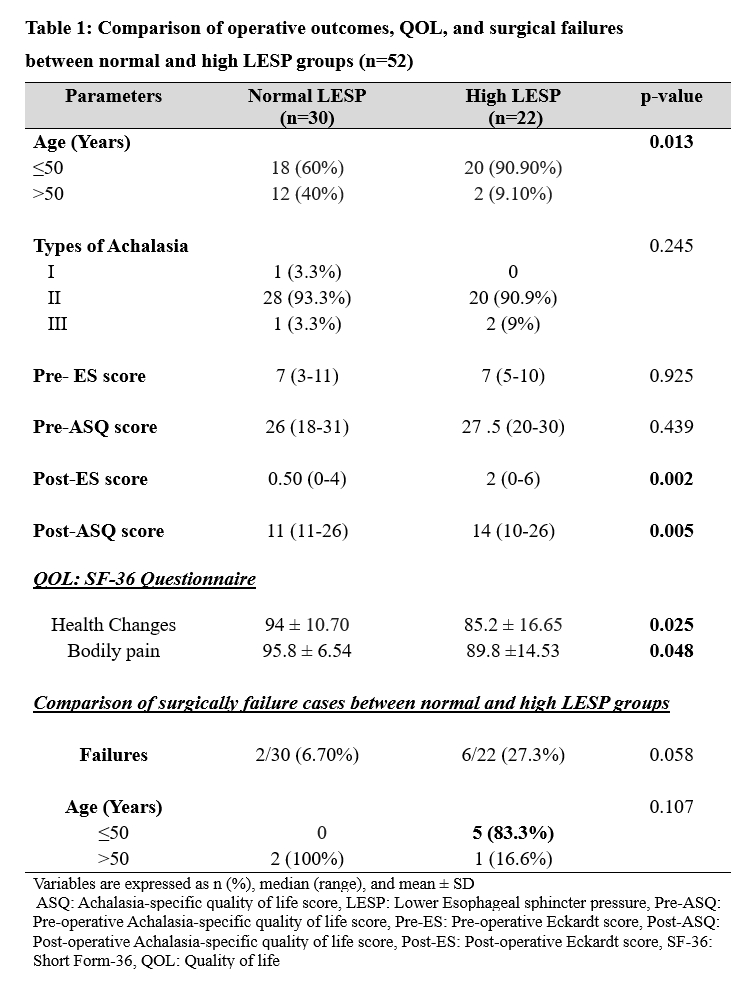
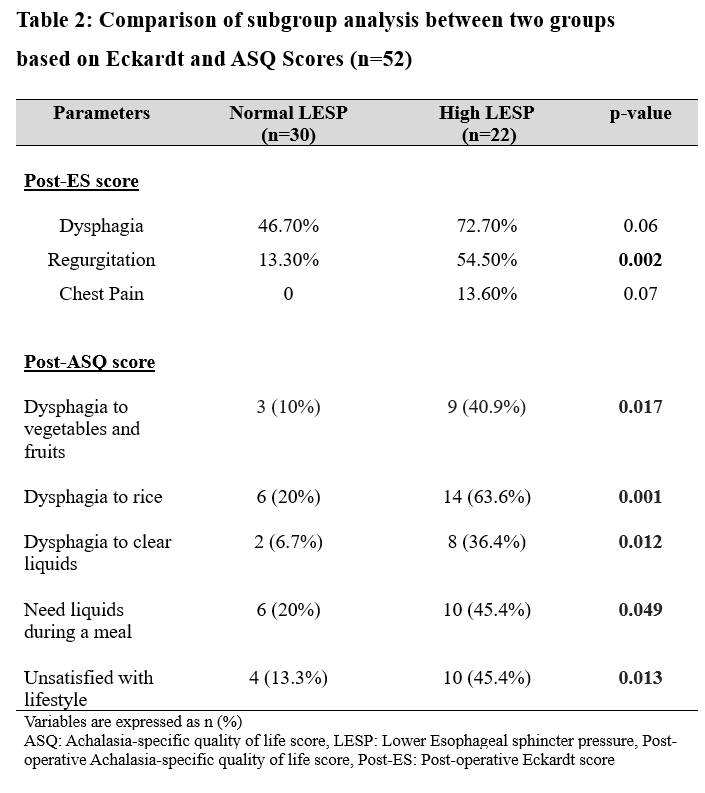
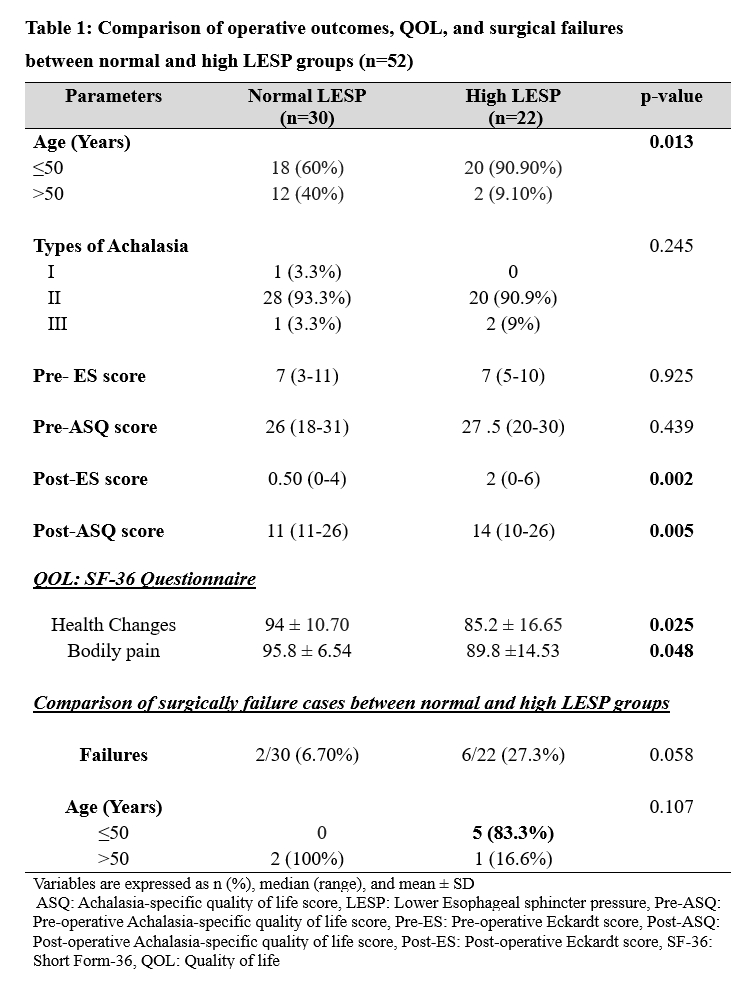
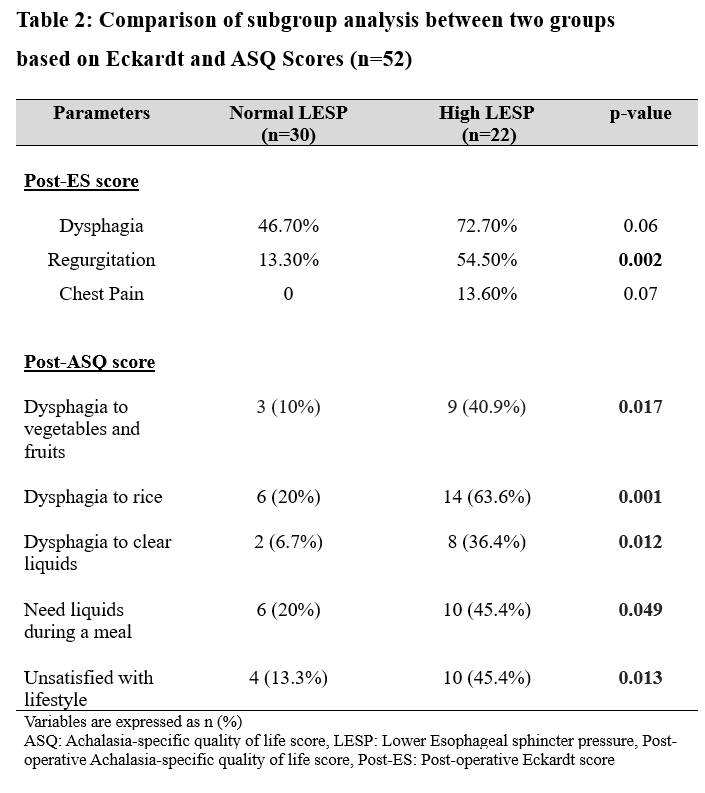
Results: The preoperative characteristics of the two groups were comparable. Among the 52 patients, the distribution of achalasia subtypes was as follows: Type I (1.92%, n=1), Type II (92.31%, n=48), and Type III (5.77%, n=3). The preoperative Eckardt and ASQ scores were similar between the groups. Notably, the high LESP group (n=22) had a significantly younger population (?50 years: 90.90% vs. 60%, p=0.013). Patients with normal LESP (n=30) experienced less severe symptoms, including dysphagia (46.7% vs. 72.7%, p=0.06), regurgitation (13.3% vs. 54.5%, p=0.002), and chest pain (0% vs. 13.6%, p=0.070) in the post-operative period. Consequently, the normal LESP group had significantly lower postoperative Eckardt scores (0.5 vs. 2.00, p=0.002) and better achalasia-specific quality of life scores (11 vs. 14, p=0.005). Additionally, the quality of life (QOL), as assessed by the SF-36 questionnaire, was significantly better in the normal LESP group. The high LESP group had a higher rate of treatment failures (27.3% vs. 6.7%, p=0.058) (Table 1).
Conclusion: High LESP may indicate more fibrotic LES, making it more challenging to completely disrupt the LES during myotomy. High LESP may be associated with persistent esophageal spasm, which can contribute to treatment failure.This subset of patient may require a more extensive and long myotomy.
Back to 2025 Posters