Back to 2025 Abstracts
RETROPERITONEAL AND LATERAL PELVIC LYMPHADENECTOMY FOR COLORECTAL NODAL METASTASIS
Kristofor Olson
*, Seija Maniskas, Makenna Marty, Jade Nguyen, Kevin Labadie, Lily L. Lai, Andreas M. Kaiser
Surgery, City of Hope, Duarte, CA
BackgroundColorectal cancer nodal metastasis to the retroperitoneum and pelvic nodes (LN) are functionally considered stage IV disease. As the approach to oligometastatic colorectal metastasis evolves, selective metastatectomy is considered the standard of care for other distant sites such as the liver and lungs. The benefit of lymphadenectomy for patients with retroperitoneal or lateral pelvic nodal metastasis remains controversial.
MethodsSingle center retrospective review of all patients who underwent resection of the primary colon/rectal cancer and corresponding resection of retroperitoneal (RP)/lateral pelvic lymph node (LP) metastasis between 2011 and July 2024. Excluded were patients with peritoneal disease, lack of followup, or missing data. "Synchronous" versus "metachronous" groups were defined as lymphadenectomy at the time of primary tumor resection versus after a disease-free interval, respectively. Recurrence free survival (RFS) and overall survival (OS) were measured from the date of lymphadenectomy and initial diagnosis, respectively. Univariate Cox regression analysis was performed to evaluate factors associated with RFS, OS, and pathologic positive lymph node metastasis (pN+).
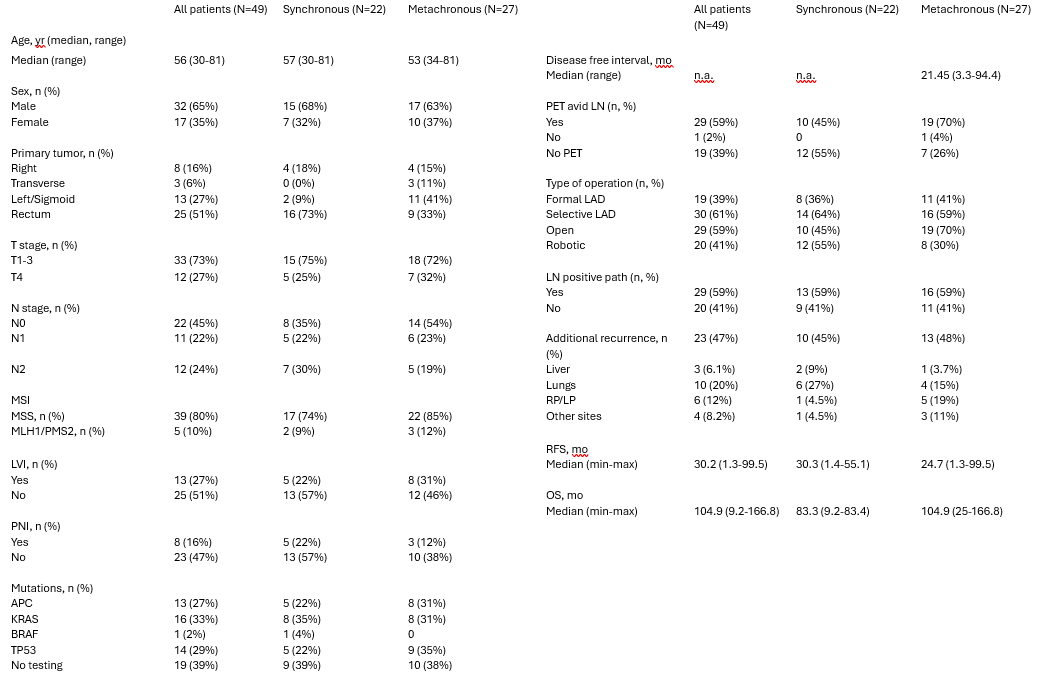
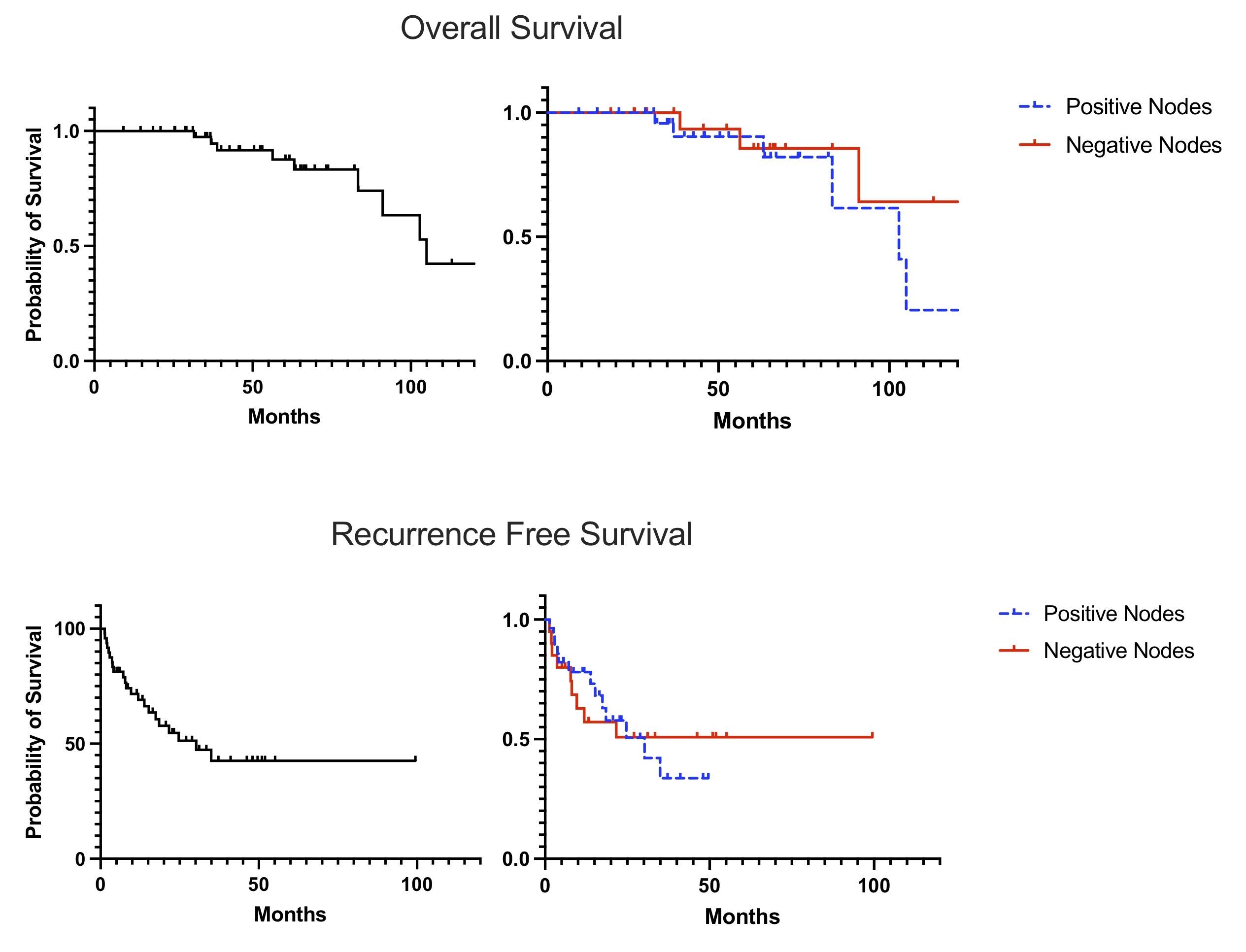
ResultsForty-nine patients (F 35%) with median age 56 (IQR 46-64) underwent RP or LP LN dissection for synchronous (47%) or metachronous (53%) metastasis. 35% of patients had other distant metastases. Primary site distribution was the right (14%), transverse (10%), left colon (27%), and the rectum (49%). Formal lymphadenectomy was performed in 19 (39%) patients, while the 30 (61%) underwent selective lymphadenectomy. Robotic-assisted procedures were performed on 41% of patients. Five synchronous and 6 metachronous patients had a concurrent hepatectomy for liver metastasis. Postoperative complications included chyle leak (4.1%), bowel obstruction (4.1%), infectious (4.1%). Final pathology revealed positive RP or PN metastasis in 59% of the synchronous patients and 59% of the metachronous patients. No variables could significantly predict lymph node positivity. Recurrent disease evolved in 47% of patients, median RFS overall was 30.2 months [range 1.2-55.1], 30.25 vs 24.7 months synchronous vs metachronous LND, respectively. Median OS for the entire cohort was 104.9 months [range 9.1-166.8], 5-year survival 87%. Pathological node positivity was not predictive of RFS or OS.
ConclusionsThe utility of selective or formal lymphadenectomy in patients with retroperitoneal or lateral pelvic nodal metastasis remains controversial but in our series was associated with a high survival rate. While node-positive patients who did not undergo lymphadenectomy were not included in this study, the lack of difference between the pN+ and pN- groups suggests that lymphadenectomy may be beneficial in appropriately selected patients with appropriate systemic disease control.
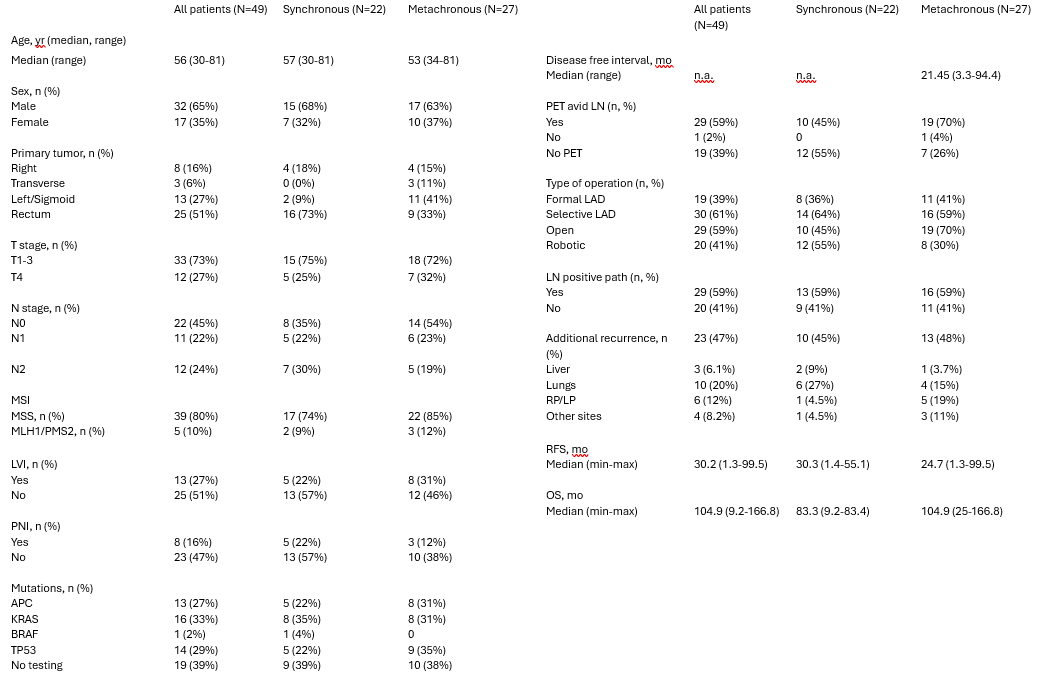
Demographic and clinicopathologic data
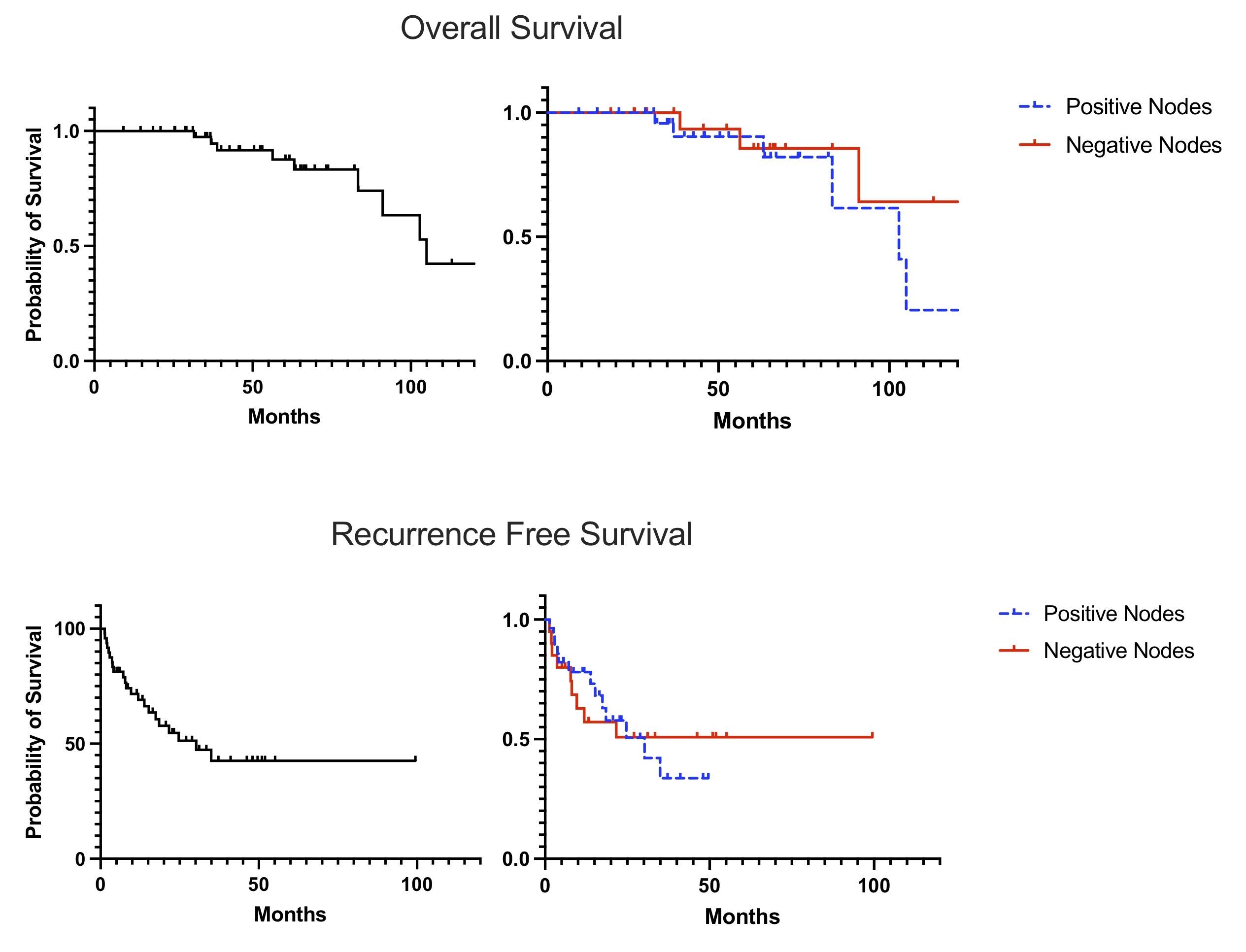
Survival graphs for entire cohort, and stratified by lymph node positivity
Back to 2025 Abstracts