Back to 2025 Abstracts
A POPULATION-LEVEL, LONGITUDINAL ASSESSMENT OF POST-PANCREATECTOMY EXOCRINE INSUFFICIENCY AND ITS FINANCIAL BURDEN FOR PATIENTS WITH PANCREATIC CANCER
Patricia Lu
*2, Yu-Hui Chang
2, Chee-Chee Stucky
2, Patricia Cronin
2, Alexandra Potter
1, George Linderman
1, Jeffrey Yang
1, Michelle A. Anderson
2, Norio Fukami
2, Douglas O. Faigel
2, Laurence Miller
2, Rahul Pannala
2, Richard Bold
2, Nabil Wasif
2, Zhi Ven Fong
21Mass General Brigham Inc, Boston, MA; 2Mayo Clinic Arizona, Scottsdale, AZ
BackgroundPost-pancreatectomy exocrine insufficiency (PEI) is a common occurrence after resection for pancreatic cancer and is treated with pancreatic enzyme replacement therapy (PERT). PERT has no generic formulations and can be very costly. We sought to characterize the out-of-pocket cost of PERT in patients with PEI after resection for cancer, and secondarily assess the association of PERT prescription and overall survival.
MethodsThe SEER-linked Medicare database was queried for all patients diagnosed with pancreatic cancer who underwent either pancreaticoduodenectomy (PD) or distal pancreatectomy (DP) from 2010 to 2019. Patients with concurrent celiac disease, cystic fibrosis, or chronic pancreatitis were excluded. PEI was defined as filling at least two prescriptions of PERT. Cumulative out-of-pocket costs were calculated per year on medication and stratified by procedure and radiation. Overall five-year survival was analyzed using a Cox proportional hazards model and Kaplan Meier curves using six months as the landmark time.
ResultsA total of 11,854 Medicare beneficiaries with resected pancreatic cancer were identified, of which 4,653 (39%) had PEI and 7,201 (61%) did not. Median age was 73.0, 50.6% were female and 83.6% White. For treatment, 25.9% underwent DP and 74.1% underwent PD; 7% received neoadjuvant radiation while 23.5% received adjuvant radiation. Logistic regression demonstrated that female sex (OR 1.25, 95% CI 1.16-1.35,
p<0.001), neoadjuvant radiation (OR 1.93, 95% CI 1.67-2.24,
p<0.001), and PD (OR 2.45, 95% CI 2.23-2.7,
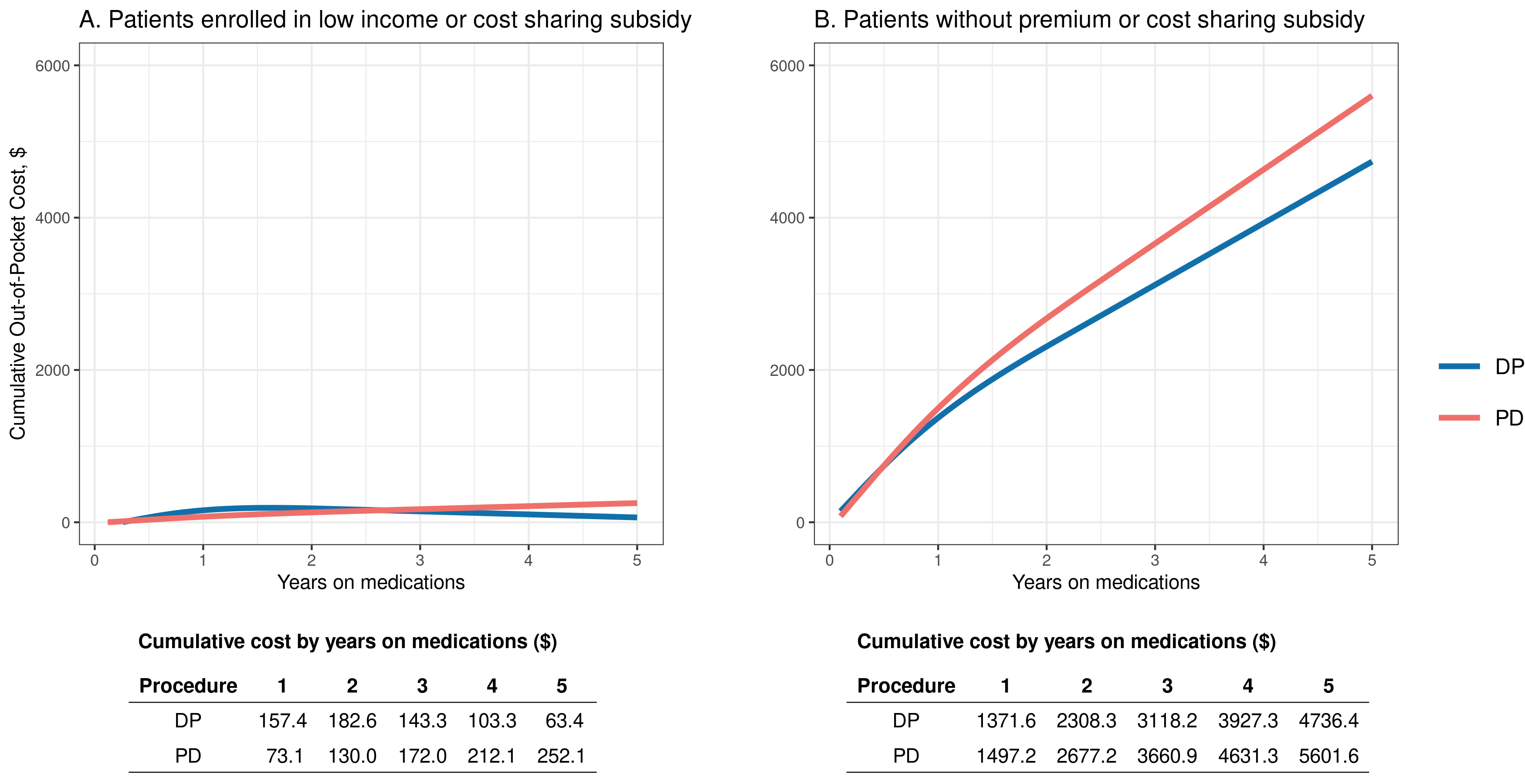
p<0.001) were risk factors for developing PEI. Of patients who had PEI, 16.3% were enrolled in a low-income or cost-sharing subsidy while 83.7% were not. Patients without a subsidy who underwent DP paid a cumulative $4,736 out-of-pocket for PERT after 5 years, those who underwent PD paid $5,601 out-of-pocket (Figure 1). Patients who filled PERT prescriptions had a significantly longer median overall survival compared to those who did not (2.9 years vs. 2.3 years,
p<0.001), suggesting the potential underuse of PERT for PEI.
ConclusionNearly 40% of Medicare beneficiaries developed PEI after resection for pancreatic cancer and is associated with significant cumulative out-of-pocket cost to patients. The association of PERT prescription filling and improved overall survival suggests the potential underuse of PERT in patients with PEI who otherwise could not afford treatment, highlighting the dire need to address the cost burden of PERT.
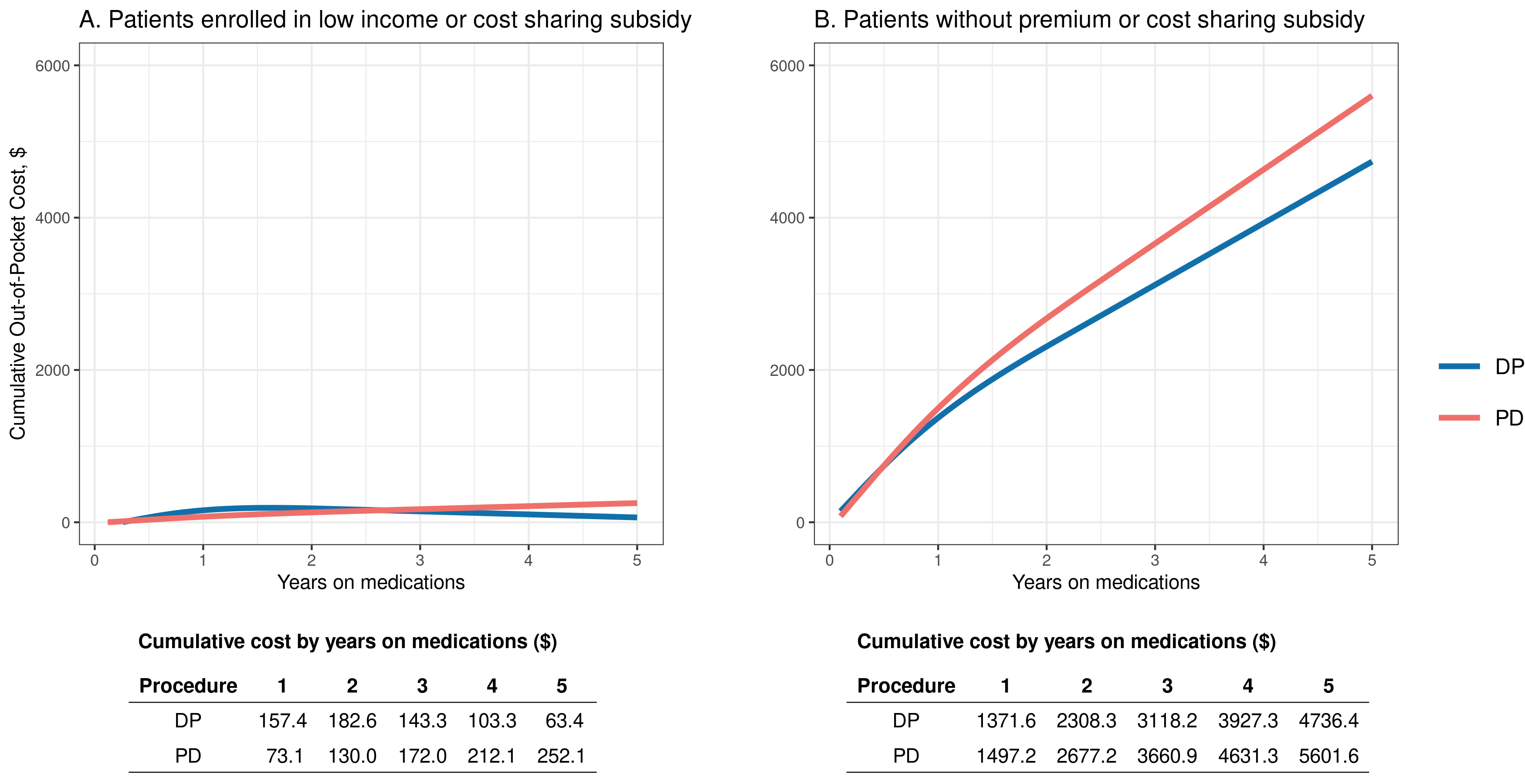 Figure 1
Figure 1. Out-of-pocket cumulative cost for PERT, by procedure
Back to 2025 Abstracts