Back to 2025 Abstracts
DEVELOPMENT AND VALIDATION OF A STRUCTURED HANDS-ON SURGICAL SKILLS TRAINING MODULE FOR OPEN DUCT-TO-MUCOSA PANCREATICO-JEJUNOSTOMY USING ANIMAL TISSUES
Rajesh Panwar
*, Siva Prasanna K, Sujoy Pal, Rashmi Ramachandran, Vuthaluru Seenu
All India Institute of Medical Sciences New Delhi, New Delhi, Delhi, India
Background: Pancreatico-jejunal (PJ) anastomosis is considered the Achilles heel of Whipple’s procedure. Simulation based training of residents for this procedure is highly desirable but not readily available. We developed a two-day training module for teaching open duct-to-mucosa PJ to the surgical trainees on an animal tissue-based simulation model. We conducted this study to validate the module.
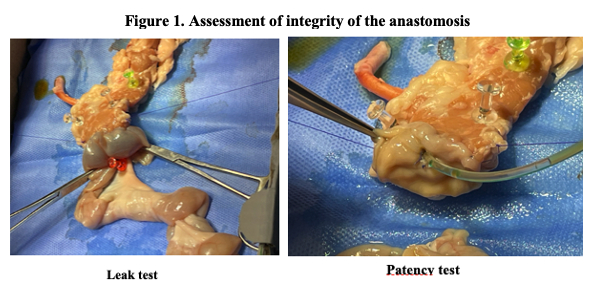
Methods: We enrolled PGY5 and PGY6 surgical trainees to participate in the course. Each trainee performed as well as assisted four PJs on the simulation model. The performance in the first case was considered baseline and the performance in the fourth case was considered as post-training. The primary outcome was the performance of the trainees assessed as per the modified Objective Structured Assessment of Technical Skills (OSATS) global rating scale. Two experts independently scored the recorded and coded videos of the trainees in a blinded manner. The final modified OSATs global score was calculated by taking average of the scores given by the two assessors. The secondary outcomes were operation time and integrity of the anastomosis as assessed by absence of leak as well as patency of the anastomosis (Figure 1). Anonymized feedback was also obtained from the trainees at the end of the course.
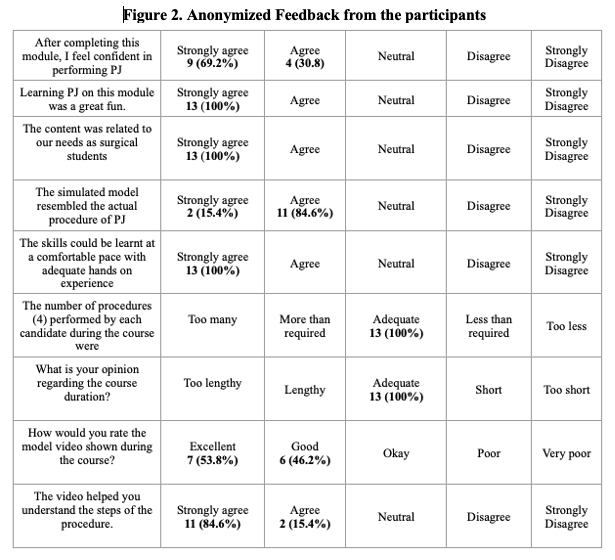
Results: Thirteen surgical trainees participated in the courses from March 2024 to July 2024. The inter-rater reliability of the two experts for the modified OSATS global score was excellent as suggested by Cronbach’s alpha of 0.828. The mean modified OSATS global score of the trainees significantly improved from 26.6 ± 2.1 in the first case to 29.1 ± 1.4 in the fourth case (p=0.001). The mean time taken to complete the procedure also significantly reduced from 41.0 ± 6.6 minutes in the first case to 26.6 ± 4.4 minutes in the fourth case (p<0.001). The integrity of the anastomosis significantly improved from 69% in the first case to 100% in the case 4 (p=0.030). All the participants provided positive feedback regarding the course. (Figure 2)
Conclusion: The open duct-to-mucosa PJ training module significantly improved the surgical skills of the trainees. It also met the expectations of the participants as suggested by the immensely positive feedback. Further studies are required to assess whether this also transforms into improvement in the operative room performance.
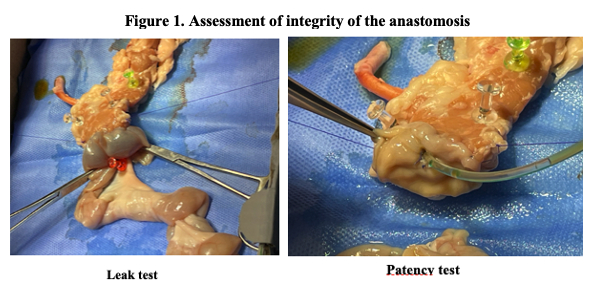 Figure 1. Assessment of integrity of the anastomosis
Figure 1. Assessment of integrity of the anastomosis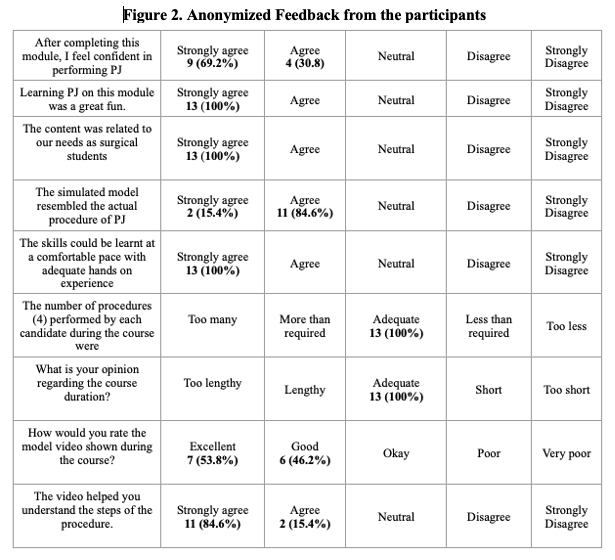 Figure 2. Anonymized Feedback from the participants
Figure 2. Anonymized Feedback from the participants
Back to 2025 Abstracts