Introduction
Achalasia is a motor disorder of the esophagus characterized by loss of peristalsis and an inability of the lower esophageal sphincter to relax appropriately, resulting in dysphagia, vomiting, chest pain, and often nutritional deficiencies. The preferred surgical techniques for treatment include Laparoscopic Heller Myotomy (LHM) and Peroral Endoscopic Myotomy (POEM). Despite improved postoperative esophageal patency, differences in perioperative weight have not been adequately studied. Therefore, we aimed to assess postoperative weight changes and clinical outcomes in patients undergoing LHM and POEM.
Methods
1,204 clinical encounters for patients with an achalasia ICD-10 diagnosis code were identified between May 2012 and May 2022. Patients without surgical intervention, weight data less than 1 year, and duplicates were excluded. Thus, 64 patients with a surgical history of POEM or LHM and weight data at 1 year and greater were retrospectively analyzed. Records for age, sex, achalasia subtype, ASA score, preoperative achalasia treatment, hospital length of stay, 30-day readmission, mortality, perioperative weight, postoperative BMI, and Eckardt scores were reviewed and compared by Pearson Chi-Squared, Fisher’s Exact Test, Mann-Whitney, and Wilcoxon test. P-values < 0.05 were considered significant.
Results
Of the 64 study patients, 52 underwent LHM and 12 underwent POEM. POEM patients had a slightly higher mean age; however, this difference was not statistically significant (65 years vs. 57.50 years; p=0.335). Otherwise, patient demographics including sex, achalasia subtype, ASA score, and preoperative comorbidities were similar between groups. Both LHM and POEM patients experienced similar hospital length of stays and rates of readmission. POEM patients had a higher BMI at their immediate postoperative visit (p=0.039) and a greater weight at 6 months (p=0.032). Weights and BMIs were comparable at subsequent time points. There were no significant differences in median Eckardt scores between groups. POEM patients had a statistically higher likelihood of requiring follow up LHM surgical intervention (p=0.007).
Conclusion
Given the short-term increase in BMI and weight gain at immediate postoperative and 6 months, respectively, POEM functions to improve esophageal patency shortly after surgery. However, compared to LHM, POEM patients were more likely to require re-intervention, suggesting that POEM may have reduced long-term durability in treating achalasia. While there was a slight worsening of Eckardt scores in POEM patients at the 2-year mark, this difference was not statistically significant. Overall, the similarity in Eckardt scores between groups may reflect the subjective nature of the scoring system and may fail to account for clinically significant differences in achalasia symptoms between postoperative LHM and POEM patients.
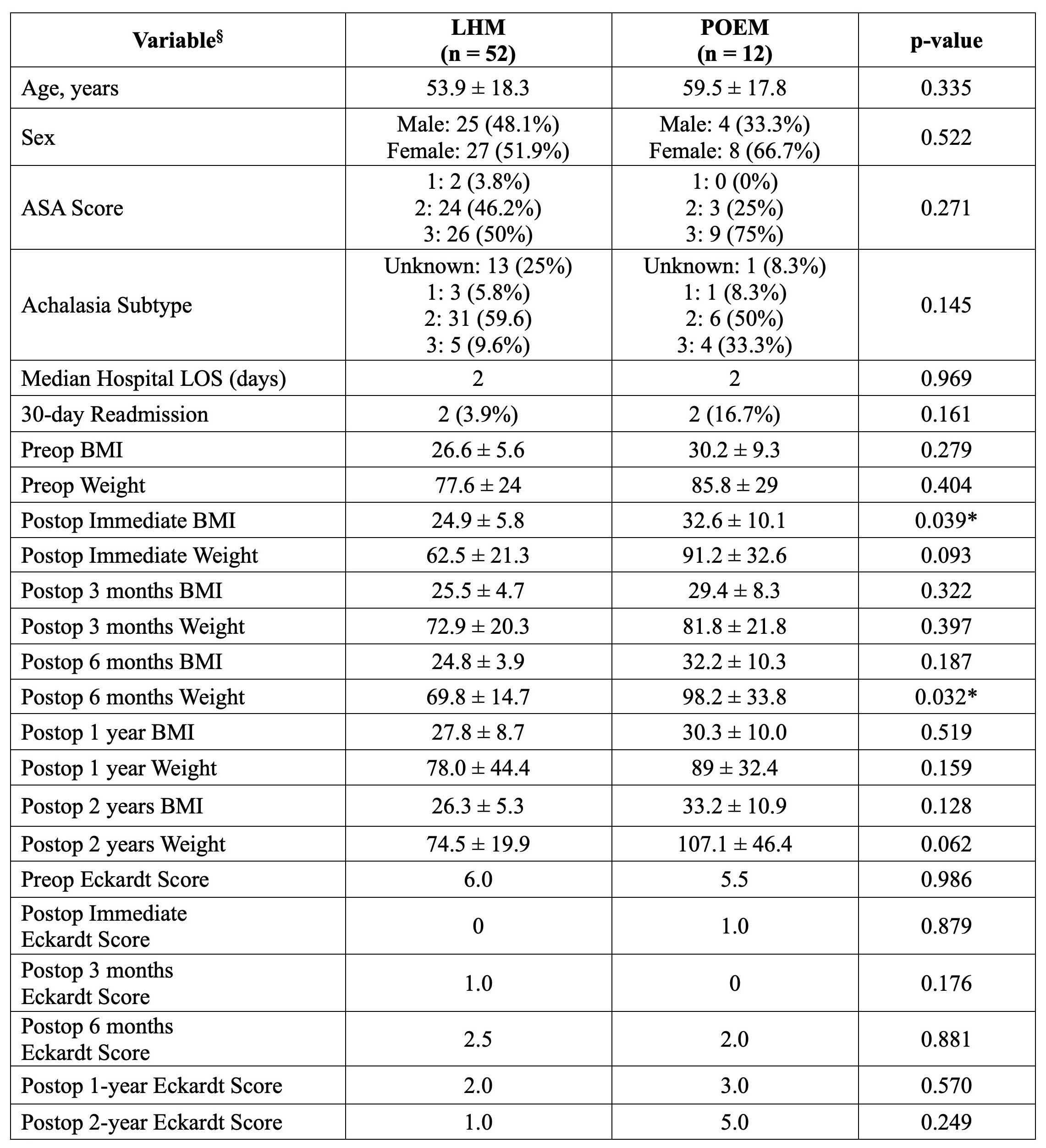
§Mean ± SEM (Standard Error of the Mean), unless otherwise stated; Weight measured in kilograms; *Statistically significant; LHM = Laparoscopic Heller Myotomy; POEM = Peroral Endoscopic Myotomy; LOS = Length of Stay; BMI = Body Mass Index; Preop = preoperative; Postop = postoperative.