Large bowel obstruction (LBO) is an uncommon complication that can arise from acute pancreatitis. Cases of chronic pancreatitis have been observed to result in small bowel obstruction (SBO), specifically in the form of groove pancreatitis. Nevertheless, the association between acute pancreatitis and duodenal obstruction is rare, and the underlying mechanism remains poorly understood.
A 36-year-old male with a history of Arnold Chiari malformation type II and gastrostomy tube feeding presented with epigastric pain that radiates to his back, weight loss, and an inability to tolerate tube feeding. His last bowel motion occurred seven days ago. The patient's vital signs were within the normal range. Initial laboratory investigation revealed leukocytosis with neutrophilic predominance, elevated C-reactive protein levels, and normal lipase levels. The abdominal computed tomography (CT) scan revealed the presence of gastric and duodenal dilation, along with an enlarged pancreatic head exhibiting peripancreatic fluid and inflammation around the pancreatic head and duodenum. Esophagogastroduodenoscopy revealed dilation in the second segment of the duodenum, with a biopsy showing duodenitis. Furthermore, attempts to advance the scope beyond this point, using both adult and pediatric scopes, were unsuccessful. A magnetic resonance cholangiopancreatography scan showed an abrupt transition point between the second and third portions of the duodenum. The patient commenced treatment for a diagnosis of pancreatitis, which improved his tolerance for tube feeding. A subsequent CT scan of the abdomen, conducted after a period of 2 months, revealed the successful resolution of duodenal obstruction with no signs of pancreatic or peripancreatic inflammatory changes.
Acute pancreatitis should always be evaluated in patients who arrive with radiographic evidence of inflammatory pancreatic changes and small intestinal obstruction. Given the concurrent remission of the patient's symptoms with the radiographic resolution of pancreatitis and SBO, the etiology of his SBO is most likely acute pancreatitis. The mechanism by which acute pancreatitis can cause duodenal obstruction is likely due to external compression, given the proximity of the pancreatic head to the second and third parts of the duodenum. It is likely that the patient's duodenitis also contributed to his obstruction. It may be possible that in acute pancreatitis, there is an extravasation of pancreatic enzymes into the duodenum, leading to the duodenitis seen in our patient. Although the concept has not been previously documented for duodenal obstruction, it has been reported in the case of large bowel obstructions caused by acute pancreatitis. More cases are needed to explore the association between acute pancreatitis and duodenal obstruction.

The EGD finding shows an obstruction observed in the second part of the duodenum. Both adult and pediatric scopes were unable to pass through this portion of the duodenum, and the procedure was termiated
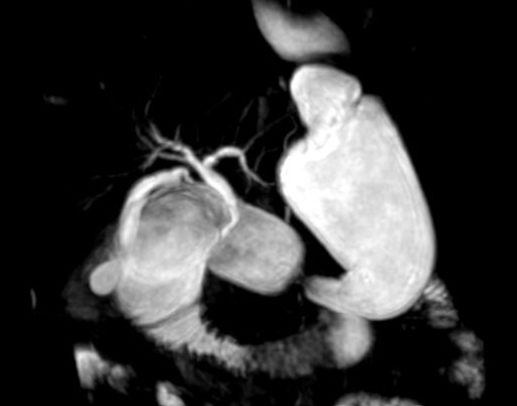
A MRCP scan showing a distended stomach and proximal duodenum with an abrupt transition point between the second and third portion of the duodenum