Background
Pancreaticoduodenectomy (PD) is the standard treatment for pancreatic head and periampullary lesions. Studies suggest that minimally invasive PD is safe and advantageous in reducing postoperative complications, but it is used less frequently in emergency settings. We aimed to assess patient-level and hospital-level factors as well as outcomes associated with the use of laparoscopic PD in emergency versus elective settings for pancreatic cancer.
Methods
We examined the National Inpatient Sample (NIS) database from 2016-2020 to retrospectively identify patients who underwent emergent and elective laparoscopic PD for pancreatic cancer using ICD-10- CM codes. Multivariable analyses were performed to assess differences in age, sex, ethnicity/race, income, insurance, Charlson Comorbidity Index (CCI), and hospital characteristics associated with mode of presentation. Surgical outcomes including length of stay (LOS), complications, expenditures, and in-hospital mortality were analyzed by mode of presentation.
Results
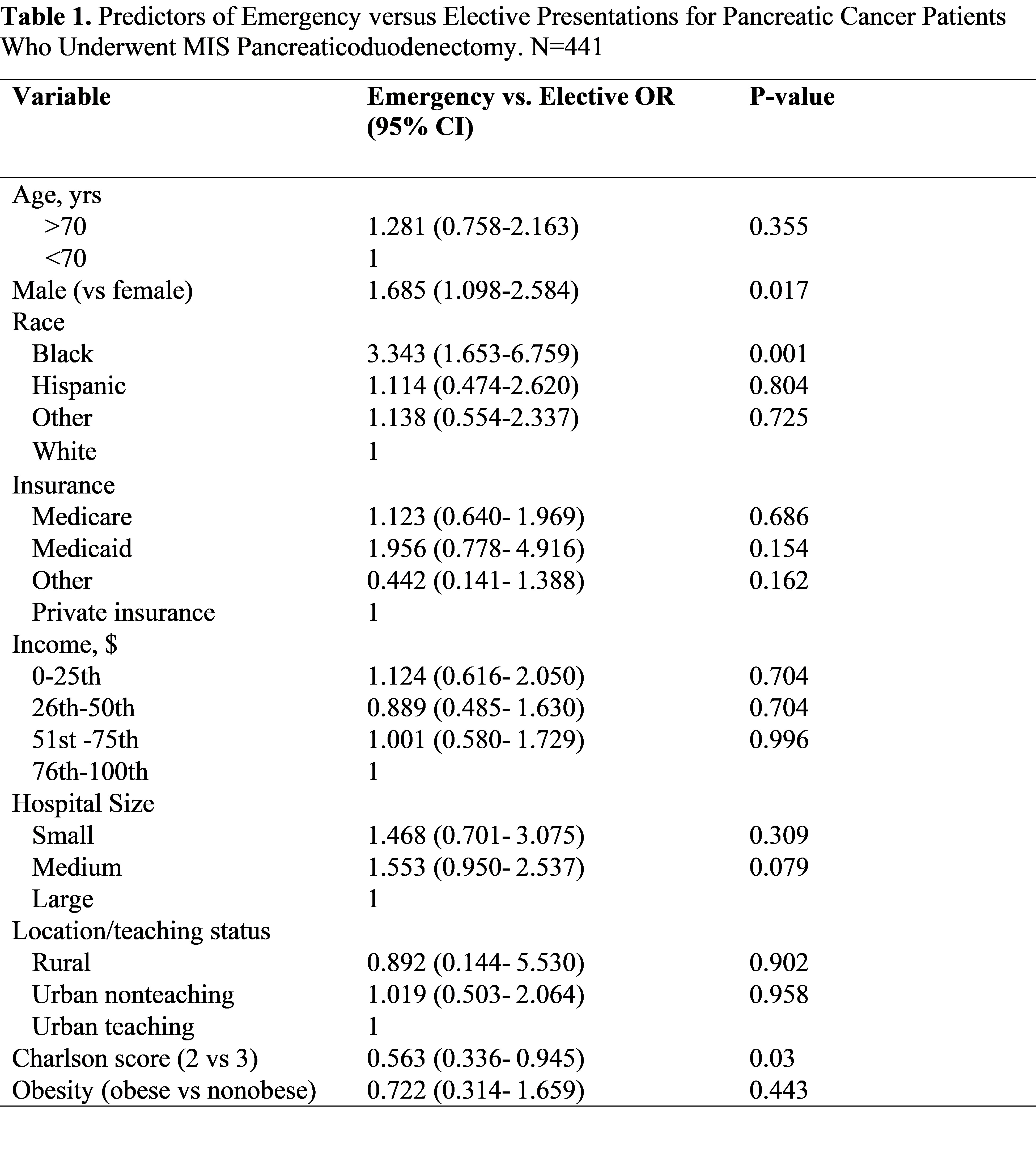
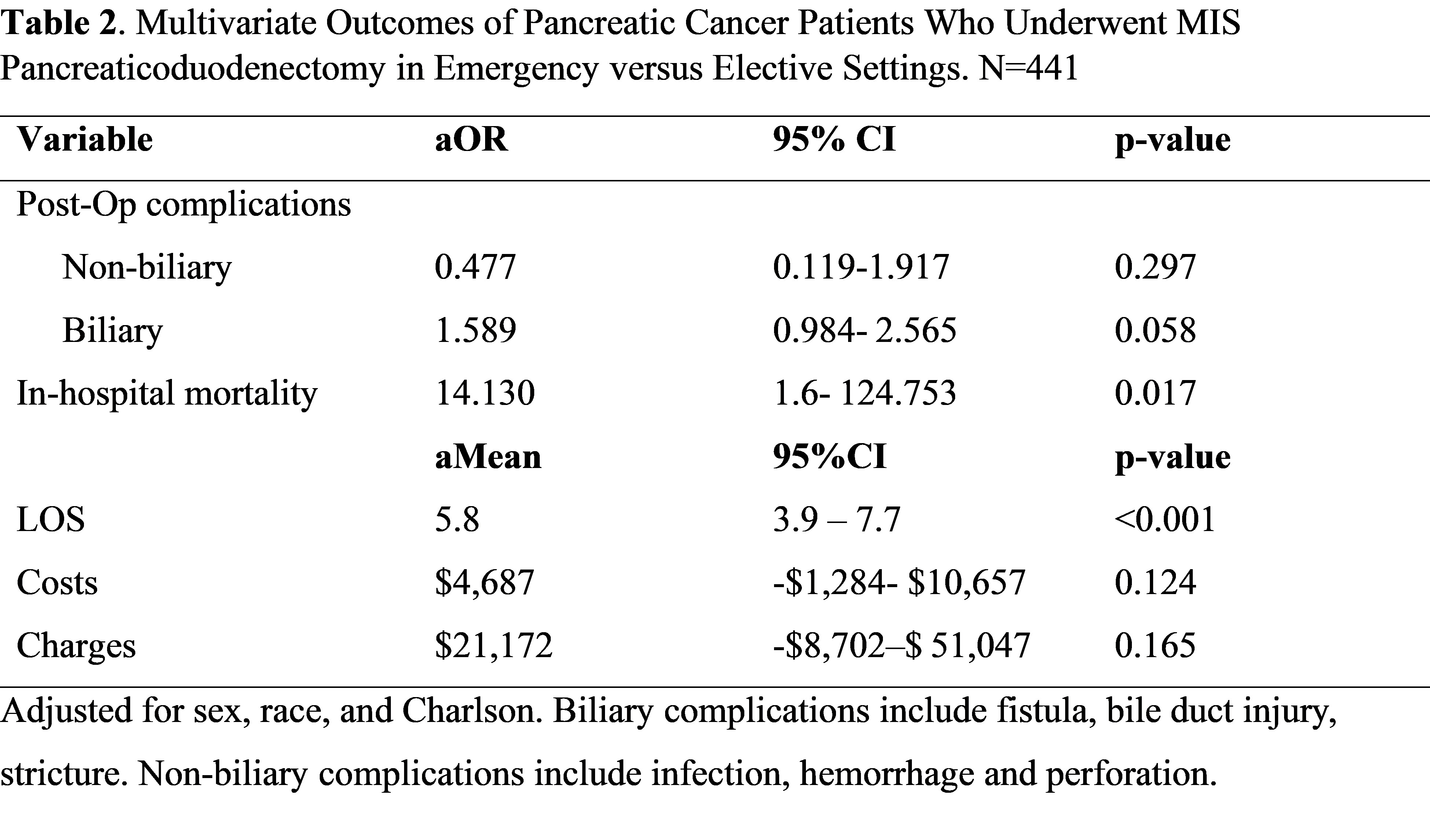
Of 441 patients identified, 245 (55.6 %) had elective surgery and 196 (44.4%) had emergent surgery. Males (60.2% versus 49.4%), African Americans (18.5% versus 6.4%) and patients with 3 or more comorbidities (84.2% versus 74.7%) were more likely to undergo surgery in emergency settings. Caucasians (76.8% versus 67.2%) and Hispanics (7.3% versus 5.8%) were more likely to be elective cases. No differences were noted by age, insurance, income, obesity or hospital size or teaching status. On multivariate analysis, emergent cases displayed a longer hospital stay by 5.8 days (p<0.001) and higher odds of in-hospital mortality (aOR: 14.1, p=0.017) compared to elective cases. No significant differences were noted in post-operative complications or hospital expenditures.
Conclusion
The use of laparoscopic pancreaticoduodenctomy in emergency pancreatic cancer presentations was more likely in Male gender, Black race, and presence of multiple comorbidities. Emergent laparoscopic pancreaticoduodenctomy was associated with prolonged hospital stay and higher in-hospital mortality, but no differences in post-operative complications or economic costs. This may suggest that these patients may have a higher baseline comorbidity burden, and as such careful patient selection is advocated.