Introduction:
Pancreatic cancer, forecasted to become the second leading cause of cancer death in the United States, is a major health concern with limited treatment options. The use of immunotherapy, a novel therapeutic avenue in late-stage pancreatic cancer, presents an area of further studies. We sought to evaluate potential disparities with immunotherapy receipt among patients with metastatic pancreatic cancer.
Methods:
A retrospective analysis of Stage IV pancreatic adenocarcinoma (PDAC) patients from the National Cancer Database (NCDB), between 2016-2019, was conducted. Kaplan-Meier and multivariable regression models were utilized on variables associated with the use of immunotherapy.
Results:
Among 53,811 patients, 331 (0.61%) received immunotherapy. Use of immunotherapy grew over the years (reference 2016: for 2017, OR 1.74, 95% CI: 1.159-2.613, p-value 0.008; for 2018, OR 1.808, 95% CI: 1.209-2.705, p-value 0.004; for 2019, OR 2.228, 95% CI: 1.509-3.29, p-value <0.001). Black or African American (OR 0.74, 95% CI: 0.601-0.882, p-value 0.019) and other minority (OR 0.224, 95% CI: 0.055-0.905, p-value 0.036) patients had a lower likelihood of receiving immunotherapy compared to Caucasian patients. Patients with commercial insurance had higher odds of receiving immunotherapy compared to the uninsured or Medicare/Medicaid. Higher income (p-value <0.001) and location in Mountain (p = 0.003) or South Atlantic region (p = 0.046) were also associated with higher chances of receiving immunotherapy (Table 1). The use of immunotherapy correlated with improved survival, with a median overall survival (OS) of 10.84 months (95% CI 0.673-9.521) compared to 4.07 months (95% CI 0.035-4.001) in the non-immunotherapy group (p<0.001).
Conclusion:
Our findings reveal significant disparities in immunotherapy access, influenced by factors such as race, insurance status, geographic location, and socioeconomic standing. These insights are crucial, and given the significant improvement of survival in the immunotherapy patients, highlight the urgency of equitable access to immunotherapy and other emerging treatments to improve outcome in the disease with a notoriously low survival rate.
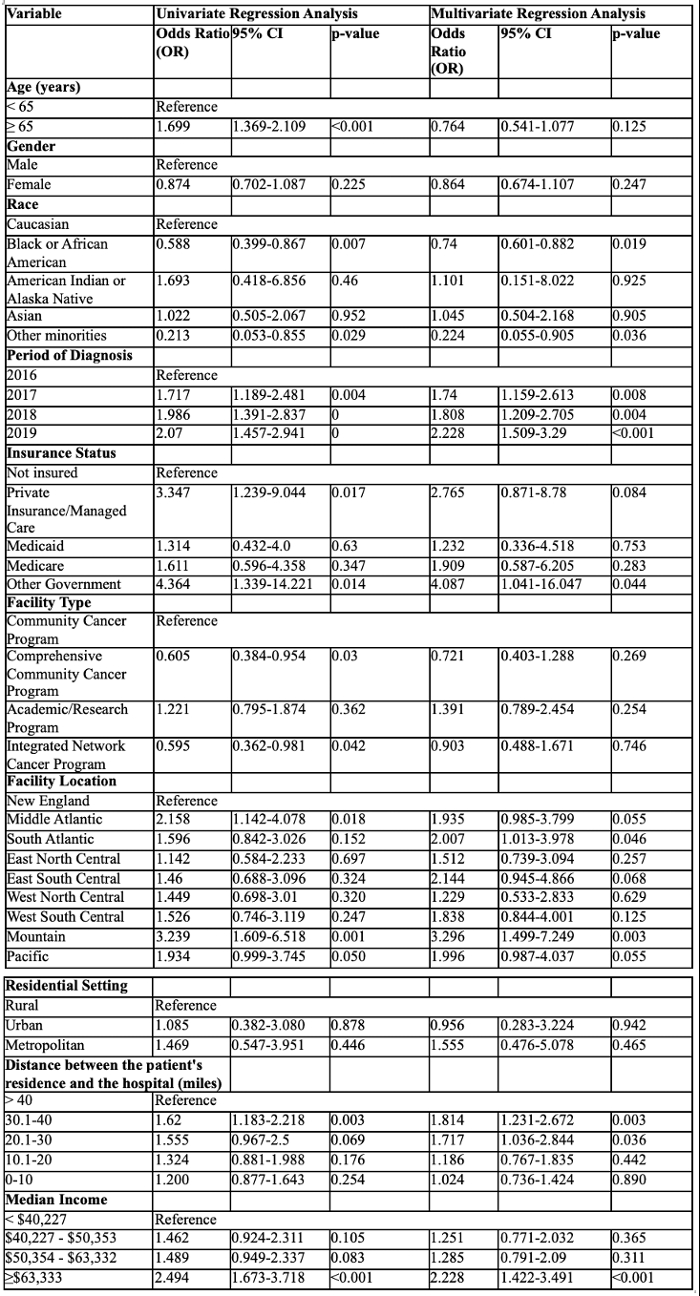
Table 1. Correlation of Patient Demographics and Clinical Characteristics with Immunotherapy Use in Stage IV Pancreatic Adenocarcinoma Patients.