Introduction: Minimally invasive distal pancreatectomy (MIDP) is increasing in utilization, and the frequency of these cases now exceeds that of the open approach. Our study aims to compare short term outcomes of RPD and LDP specifically for pancreatic ductal adenocarcinoma (PDAC) using a national database of hospital-based cohorts over a course of ten years.
Methods: The National Cancer Database (NCDB) was utilized to identify patients with PDAC who underwent distal pancreatectomy from 2010-2020. Outcomes included short term surgical and technical oncologic outcomes such as margin status and nodal harvest. Propensity-score matching (PSM) was performed comparing LPD and RPD cohorts. Multivariate logistic-regression models were then used to assess the impact of institutional volume on the MIDP surgical and technical oncologic outcomes to assess the impact of institution volume on outcomes of MID.P
Results: 1,537 patients underwent MIDP with curative intent. Most cases were laparoscopic (74.4%, 1144). There was a gradual increase in robotic utilization, from 8.7% of MIDP cases in 2010 to nearly one third (32.0%) of MIDP cases ten years later. Of all MIDP, 21.0% (n=323) were converted to open. Surgical oncologic outcomes of MIDP include a 12.7% positive margin rate and a mean of 15.4±10.1 nodes retrieved. The mean length of stay was 6.2 days, with a 7.7% unplanned 30-day readmission rate. The 30-day and 90-day mortality rates were 1.4% (n=22) and 2.9% (n=44), respectively.
After PSM, 319 pairs of patients were matched from the LDP and RDP groups. The odds of conversion to an open case was 61% less in RDP (12.3%) compared to LDP (26.3%) with no statistically significant difference in the odds of a technical oncologic results (Figure 1). There was no difference in length of stay (OR=1.0 [0.5-1.8]), 30-day readmission rate (OR=1.4 [0.8-2.4]), 30-day mortality (OR=0.8 [0.2-3.0]) and 90-day mortality (OR=1.0 [0.4-2.4]) between RDP and LDP.
When the comparing impact of the annual case volume quartiles of all MIDP cases to technical outcomes, there was no difference in the conversion to open rate (p=0.32), length of stay (p=0.67), 30-day unplanned readmission (p=0.825) and 90-day mortality (p=0.11) based on the center’s annual case volume of MIDP. However, a higher annual case volume (>12 cases per year) was associated with increased nodal harvest (p<0.01), reduced rate of R1 resection (p=0.01) and an improved rate of initiation of adjuvant systematic therapy (p=0.05) (Figure 2).
Conclusion: Laparoscopic and robotic distal pancreatectomy have similar peri- and post-operative surgical and oncologic outcomes, with a higher rate of conversion to open in the laparoscopic cohort. The rate of technical oncologic success appears improved with higher annual case volume of minimally invasive distal pancreatectomy.
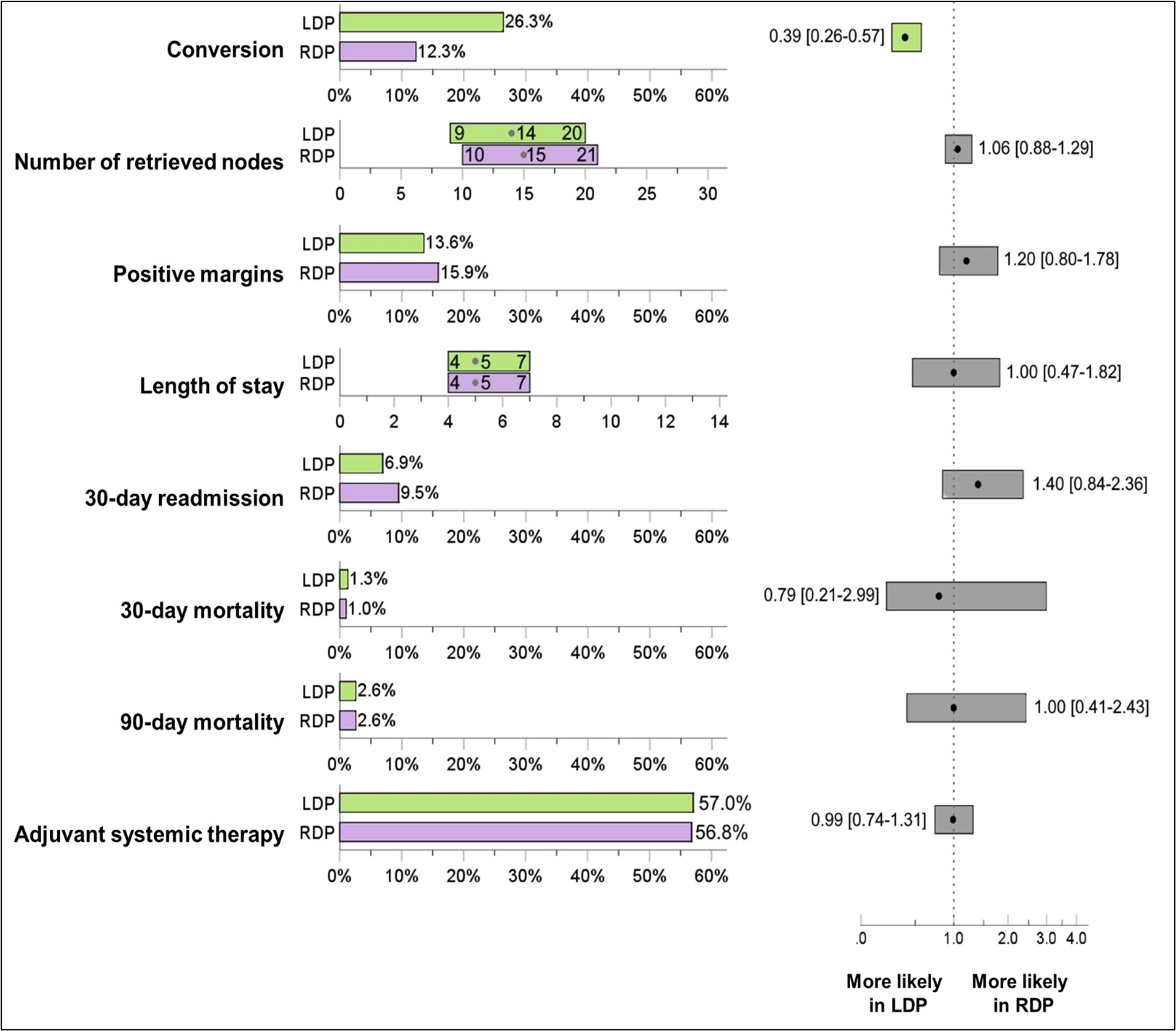
Figure 1: Comparison of short-term quality outcomes between the matched LDP and RDP groups. LDP: Laparoscopic Distal Pancreatectomy; RDP: Robotic Distal Pancreatectomy.
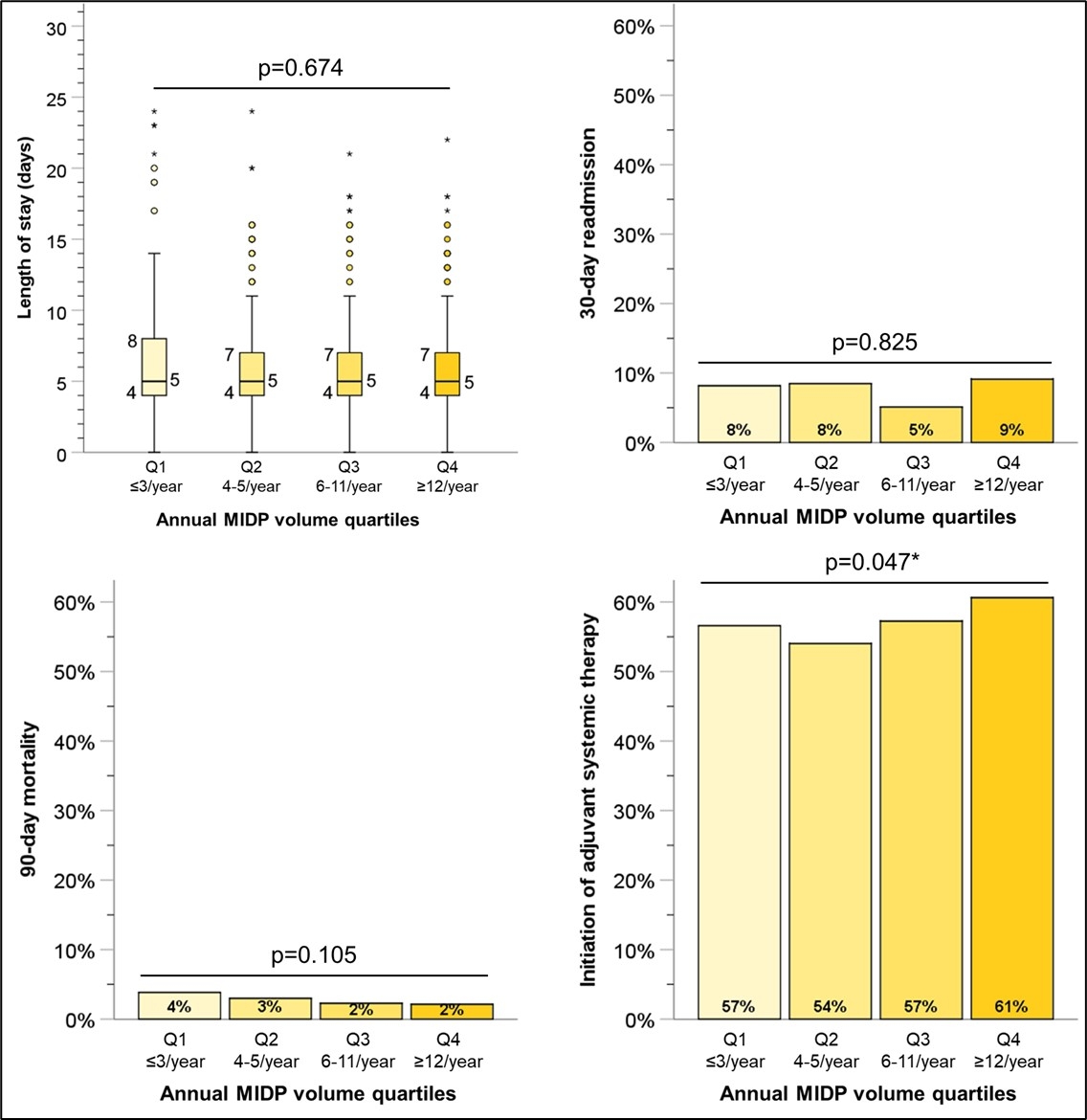
Figure 2: Impact of annual institutional MIDP volume on postoperative metrics. MIDP: Minimally Invasive Distal Pancreatectomy. * Statistically significant.