Background
Pancreatic cancer incidence and life expectancy are on the rise. Older patients are being evaluated for surgical interventions for both malignant and benign pancreatic lesions. There is a paucity of data regarding differences in outcomes of pancreatic surgery (PS) in patients 90 years of age an above when compared to their younger counterparts. We aim to evaluate in-hospital outcomes of patients undergoing pancreatic surgery according to different age groups specifically in those age 90 and older.
Methods
Retrospective cohort study of the 2016-2019 National Inpatient Sample (NIS) using ICD10-CM/PCS codes to identify patients discharged after undergoing same admission PS. Patients were subdivided into four age groups: 1) ?60 years of age; 2) 61-65 years of age and 3) 76-89 and 4) ?90 years of age. Primary outcomes were: mortality, morbidity (mechanical ventilation / shock) and post-operative complications including shock, wound dehiscence and infection. Secondary outcomes were: length of stay (LOS), health-care related charges and costs adjusted to inflation according to the price consumer index to the year 2019. Multivariate regression analysis adjusted for patient and hospital characteristics was performed for the primary and secondary outcomes.
Results
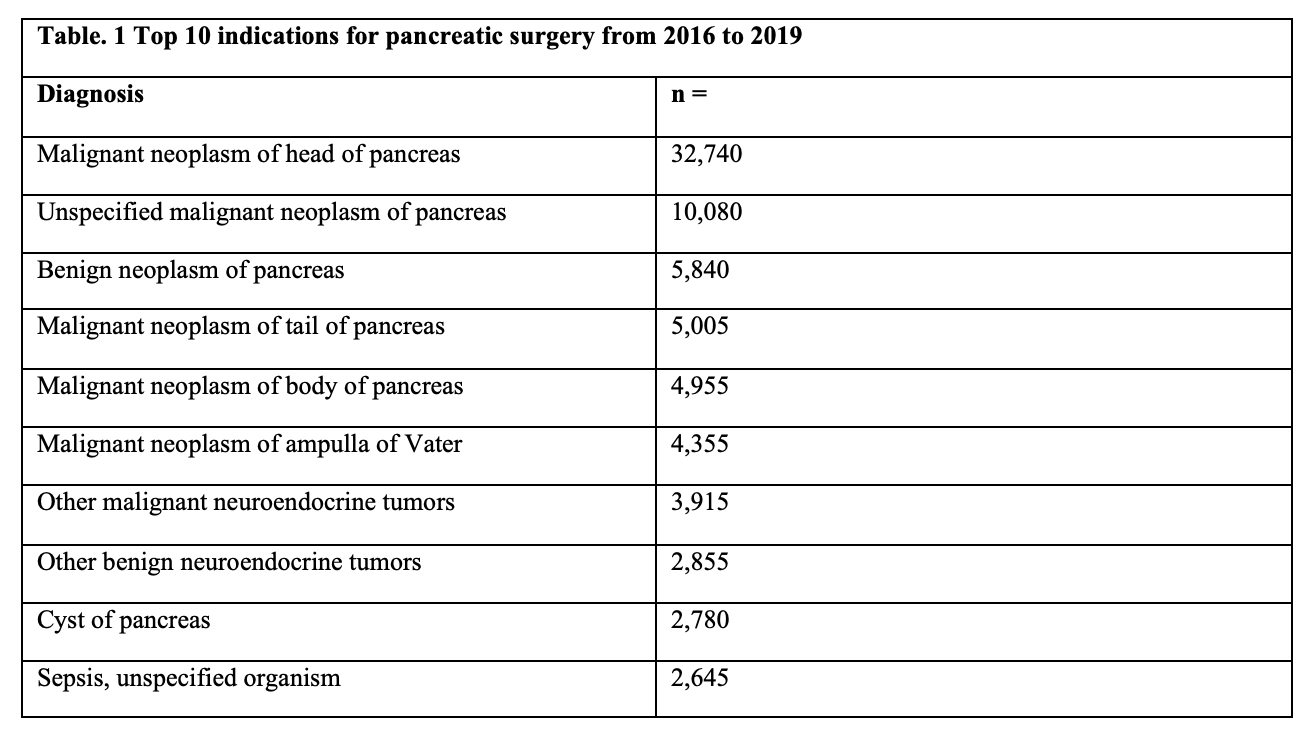
A total of 97,495 PS were identified in the study period out of which 0.87% (N=849) were performed in patients 90 years of age and above. 61.7% (N=524) of patients in this group underwent PS for a malignant neoplasm of the head of the pancreas. The top ten indications for PS are displayed in Table 1. In the nonagenarian group more than 70% of these patients were Caucasian females with Medicare as primary payer with a higher Charlson Comorbidity Index Score. They had significantly lower rates of post-operative shock (0% vs. 0.11% vs. 0.10% vs. 0.01%, P<0.01) with no differences in the rates of post-operative wound dehiscence and infection. After adjusting for confounders nonagenarians did not have increased odds of in-hospital mortality after PS [adjusted odds ratio [aOR] 1.47; 95% confidence interval [CI] 0.41-5.28)], requirement of mechanical ventilation [aOR 1.00], in-hospital shock [aOR 0.73; (0.08-6.07), post-operative shock [aOR 1.00], wound dehiscence [aOR 1.00) and post-operative infection [aOR 1.16; (0.15-8.92)]. These patients did not have higher LOS [adjusted days 0.63; (-1.37-2.65)], health-care related charges [aUS.161; (-18,621- 76,945)] and costs [aUS,494; (-2,955-19,944)].
Conclusion
Nonagenarians do not have increased mortality or worse post-operative outcomes when compared to their younger counterparts. Pancreatic head malignancy is the primary indication for these patients to undergo PS and our results show that age alone should not be an exclusive factor when offering therapeutic options to this set of patients.