Introduction:
In the wake of the RELIEF trial published in 2018, pancreatic surgeons were prompted to evaluate the effect fluid therapy has on their patients given septic complications such as anastomotic leak was found in higher frequency with those receiving restricted volume of fluids. In the following years, meta-analyses and systemic analyses have debated if fistula formation, among other complications, could be curbed by intentional fluid resuscitation during and after pancreatic resection. By adjusting fluid volume by body surface area and examining fluid balance at multiple time points, we hope to further examine this relationship.
Methods:
The study is a retrospective cohort study utilizing institutional data approved by the IRB. Adult patients with pancreatic adenocarcinoma who underwent surgical resection from December 2016 to September 2023 were evaluated. 77 patients met inclusion criteria. Electronic medical records were reviewed for fluid balance immediately finishing surgery, at 24 hours, 48 hours, and 72 hours in addition to preoperative albumin, weight, and height. Patients without this information were excluded. Fluid balance was adjusted by body surface area (BSA) via the Takahira formula to ml/m2. Demographic information in addition to tumor characteristics, treatment choices, and patient outcomes were also collected. Analysis was completed with SPSS v.27 and reviewed by a statistician.
Results:
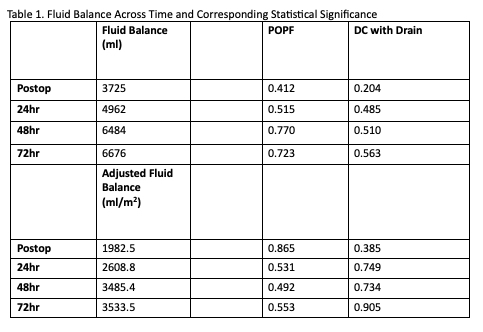
A total of 77 patients underwent pancreatic resection at an average age of 64.7 years. The majority (77.9%) of procedures conducted were pancreatoduodenectomy and the average LOS was 8.64 days. Median estimated blood loss was 250ml. The median fluid balance immediately postoperatively (3725ml), at 24 hours (4962ml), 48 hours (6484ml), and 72 hours (6676ml) was then adjusted by BSA. 5 patients (6.5%) were diagnosed with postoperative pancreatic fistula (POPF) grade B or C. Kruskal-Wallis test was used for analysis. POPF was not statistically correlated with fluid balance at measured time-points, nor was reoperation or discharge home with drain. This was calculated using both adjusted and raw values of fluid balance. See Table 1 for respective p-values. Preoperative albumin (within 30 days prior to surgery) was assessed for independent correlation with POPF in our patients with p=0.235 also demonstrating no significant difference.
Conclusion:
POPF occurrence does not correlate with fluid administration by volume or when adjusted to BSA. This supports previous research and relays the importance of further investigation on the etiology of pancreatic leak.