BACKGROUND
Pancreatic fistula is a potential complication of pancreatic surgery. The pancreas-to-spleen attenuation ratio (P/S) and pancreas minus spleen attenuation difference (P-S) can be measured with computer tomography (CT) scans and have been correlated with histologically confirmed pancreatic steatosis. We aimed to determine the association between pancreatic fat and post-operative pancreatic fistula (POPF).
METHODS
Patients who underwent major pancreatic surgery at our tertiary care center between 1999 and 2021 were included. Patients with total pancreatectomies were excluded. Pancreatic fat was measured histologically by two blinded pathologists and reported as percentages of total pancreatic parenchyma. The P/S and P-S were measured by a gastrointestinal radiologist using CT scans obtained within six months before surgery. The primary outcome was the development of a POPF within six months of surgery. A POPF was defined as a Grade B or C pancreatic fistula. Pearson correlation was used to determine the correlations between pancreatic fat. Wilcoxon rank and Fisher exact tests were performed to determine associations with POPF. Given the small sample size, a p-value < 0.10 was defined as statistically significant.
RESULTS
97 patients were included (median age 67.9 years and BMI 26.4 kg/m2; 50.5% male). Table 1. Major pancreatic surgeries included pylorus-preserving pancreaticoduodenectomy (39, 40.2%), and standard (22, 22.7%), distal (27, 27.8%), or central pancreatectomy (9, 9.3%). A total of 26 patients (26.8%) developed a POPF at 6 months. A higher BMI (29.7 vs 25.7 kg/m2, p=0.003), obesity (50.0% vs 25.4%, p=0.028), and soft pancreatic consistency (92.3% vs 40.9%, p=0.001) were associated with POPF. Patients with poorly differentiated pancreatic neoplasms had a lower frequency of POPF (8.7% vs 36.2%, p=0.014). A longer operative time (323 vs 237 minutes, p=0.107) and absence of neoplasia (21.7% vs 6.9%, p=0.109) had a trend to significance with POPF. Pancreatic fat, measured histologically or radiographically, were not significantly associated with POPF, and not significantly different based on sex or correlated with age and BMI. Tables 2 and 3. P/S and P-S were strongly correlated with pancreatic septal and total fat, p <0.001, and P-S with pancreatic intralobular fat, p<0.01. Table 3. Only pancreatic intralobular fat was significantly correlated with a soft pancreas, p<0.05.
CONCLUSION
Although a higher BMI was strongly associated with POPF, pancreatic steatosis, measured histologically and radiographically, were not. The P/S and P-S were strongly correlated with histological pancreatic septal and total fat.
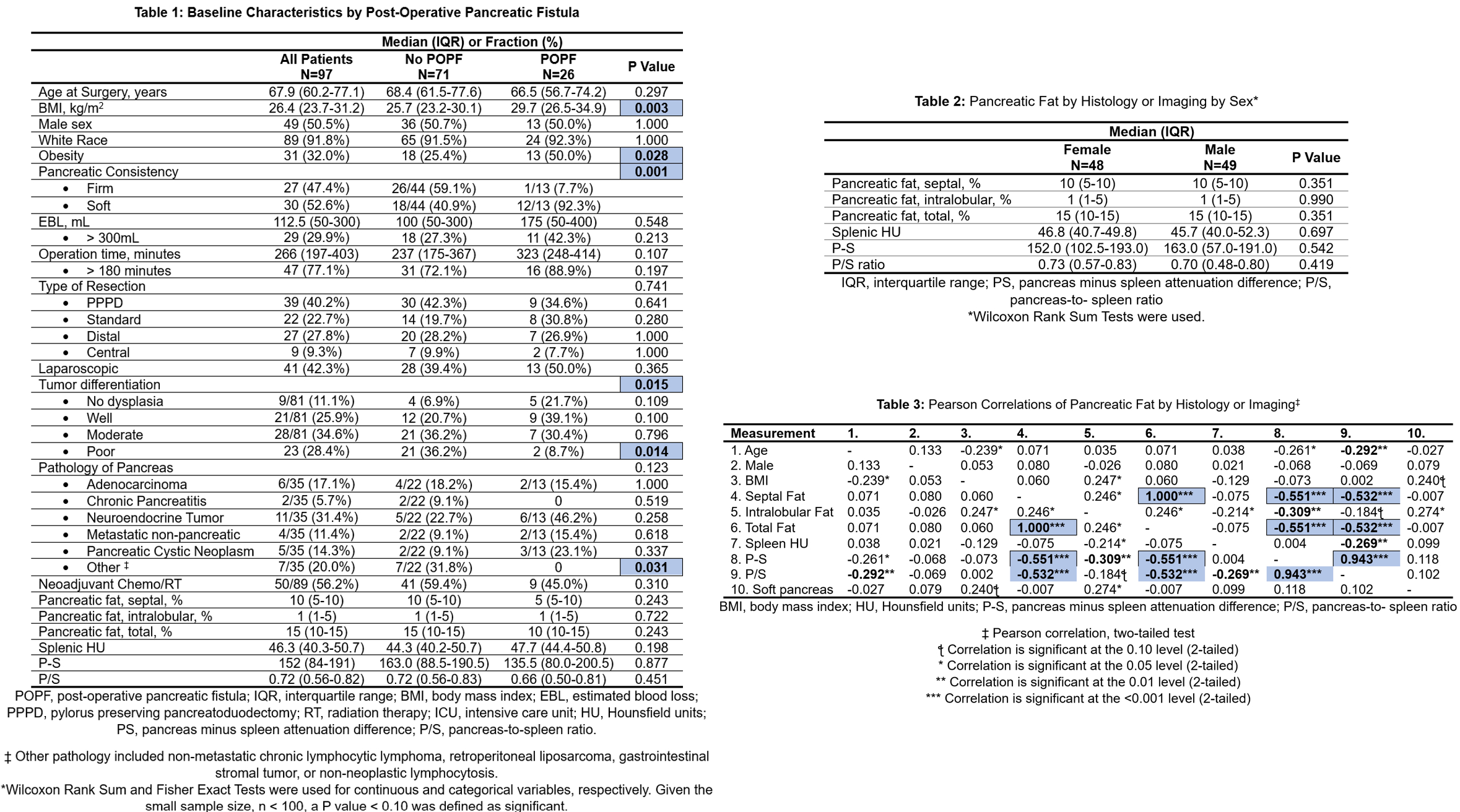
Figure 1: Baseline Characteristics by Post-Operative Pancreatic Fistula, and Pearson Correlations of Pancreatic Fat