Introduction: Different presenting symptoms, tumor location, time from symptom onset until diagnosis, and time to referral center consultation may affect outcome in patients with PDAC.
Methods: Clinical data were prospectively collected from a cohort of 671 patients in our pancreas referral center (Oct. 2018 – Sep. 2023). Descriptive statistics, X2, t-tests, linear regressions and Cox Regressions for Overall Survival (OS) were utilized.
Results: M/F ratio was 1.2/1 and median age was 66 (58-73) years. Symptoms preceded diagnosis in 91%, whereas in 9% PDAC was an incidental finding. The most common presenting symptoms were abdominal pain (35%), new onset diabetes mellitus-DM (33%), obstructive jaundice-OJ (23%), back pain (15%), weight loss (14%), fatigue (5%), steatorrhea (3%), bloating (2%), anorexia (2%) and acute pancreatitis (1%).
The most common location was the head (36%), followed by the body (31%), uncinate process (20%), tail (11%) and neck (10%). New onset DM occurred in 33% of patients 5 (3-10) months before diagnosis of PDAC. Time from symptom onset to diagnosis (Interval-1) was 2 (1-4) months and from diagnosis until referral to a pancreas specialist (Interval-2) was 1 (0-3) month. Interval-1 was significantly shorter in female patients, OJ, and location in the head, but significantly longer in male patients, weight loss, steatorrhea, new onset DM and location in the tail. Interval-2 was significantly shorter in female gender, worse ECOG-PS, new onset DM and family history of PDAC. Conversely, it was significantly longer in male gender and history of fatigue.
At diagnosis, 24% of PDACs were upfront resectable, 11% borderline resectable, 28% locally advanced, and 35% metastatic. Head tumors were significantly associated with OJ (<0.001) and were diagnosed at earlier stages than body/tail (<0.001). Body/tail tumors were more frequently metastatic at presentation (<0.001) and were significantly associated with non-specific symptoms [abdominal/back pain (<0.001), weight loss (0.023)]. Median OS of all patients was 13 (range: 1-67) months. Higher stage, PDAC in the pancreatic tail, worse ECOG-PS, anemia and longer Interval-2 were associated with worse OS.
Conclusion: This study elucidates the effect of the type of presenting symptoms, tumor location, delay in diagnosis and delay to referral to a pancreas center on the overall survival of PDAC patients.
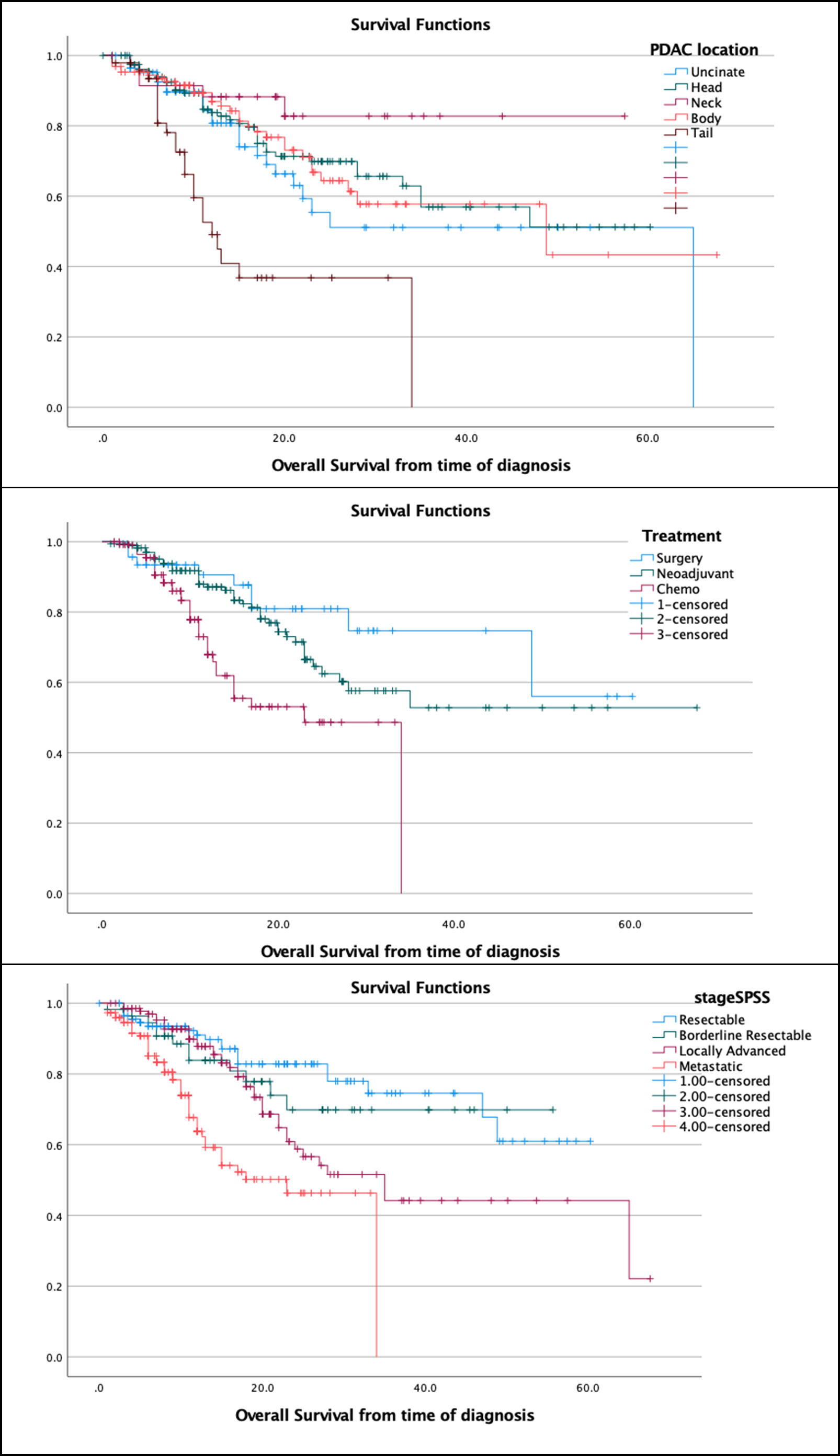
Figure 1: Kaplan-Meier curves depicting the patient overall Survival (in months) according to (a) location of the PDAC, (b) treatment and (c) stage at initial diagnosis.