BACKGROUND
Pancreatic fistula is a potential complication of pancreatic surgery. Several risk factors of post-operative pancreatic fistula (POPF) have been described, including having a soft pancreas, the surgical techniques involved, and a longer operative time. We aimed to derive a risk score of variables known at the time of pancreatic surgery to predict a POPF.
METHODS
Patients who underwent pancreatic surgery at our tertiary care center between June 1995 and March 2019 were included. Patients with total pancreatectomies were excluded. Demographics, laboratory values, and clinical data were collected retrospectively. The primary outcome was the development of a POPF within six months of surgery. A POPF was defined as a Grade B or C pancreatic fistula. Wilcoxon rank and Fisher exact tests were used to determine associations with POPF. Multivariable logistic regression with bootstrap resampling was used to derive a risk model with the best discrimination to predict a POPF. A calibration evaluation of the risk model was performed of patients without missing data. Points were assigned to each variable in the risk model based on their weighted odds ratio.
RESULTS
A total of 1,283 patients (median age 66.6 years, male 49.1%) were included. 144 patients developed a POPF. A higher body mass index (BMI) (28.3 vs 26.4 kg/m2, p<0.001), type of surgery performed (p<0.001), a longer operative time (5.27 vs 4.39 hours, p<0.001), and smaller pancreatic duct (PD) (2 vs 3 mm, p <0.001) were strongly associated with POPF. Figure 1. In multivariable logistic regression analysis, adjusting for age, male sex, white race, active smoking status, and ASA class, the strongest predictors of POPF were BMI (1.056 per 1 kg/m2, p<0.001), and PD size (0.56 per 1 mm, p<0.001). Given the large number of patients with missing data on PD size, the variable was not included in the final model. A four variable risk model of known variables with the best discrimination, called the CB2D score, was derived. The variables in the model were history of chronic pancreatitis (OR 2.57, p=0.004), history of bowel resection (OR 1.94, p=0.004), BMI (OR 1.05 per 1 kg/m2, p=0.004), and distal pancreatectomy (OR 0.54, p=0.006. Figure 2. At the lowest sextile of the risk score, the observed rate of POPF was 3.8%, whereas at the highest sextile, it was 19.0% (risk ratio: 5.03, p < 0.001). The area under the curve (AUC) of the risk score was 0.647 (95% CI: 0.588-0.707).
CONCLUSION
In this single-center large retrospective study, we derived a four-variable risk score, called the CB2D score, of known variables prior to surgery to predict POPF. The model includes, 1) history of [C]hronic pancreatitis, 2) history of [B]owel resection, 3) [B]MI, and 4) having a [D]istal pancreatectomy. This simple risk score may help to predict patients at high risk of POPF. Further external validation is recommended.
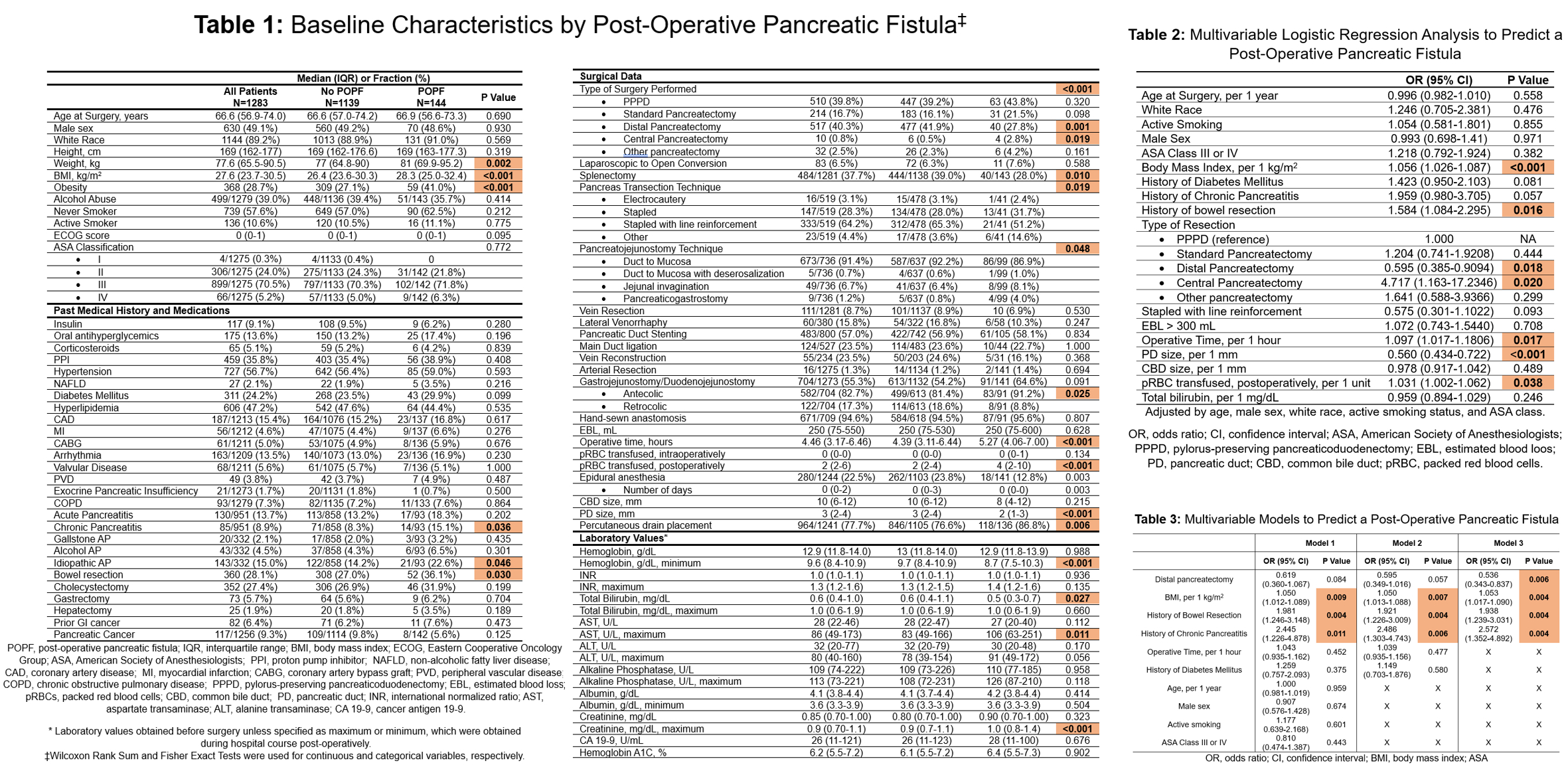
Figure 1: Baseline Characteristics and Multivariable Logistic Regression Analysis to Predict a Post-Operative Pancreatic Fistula
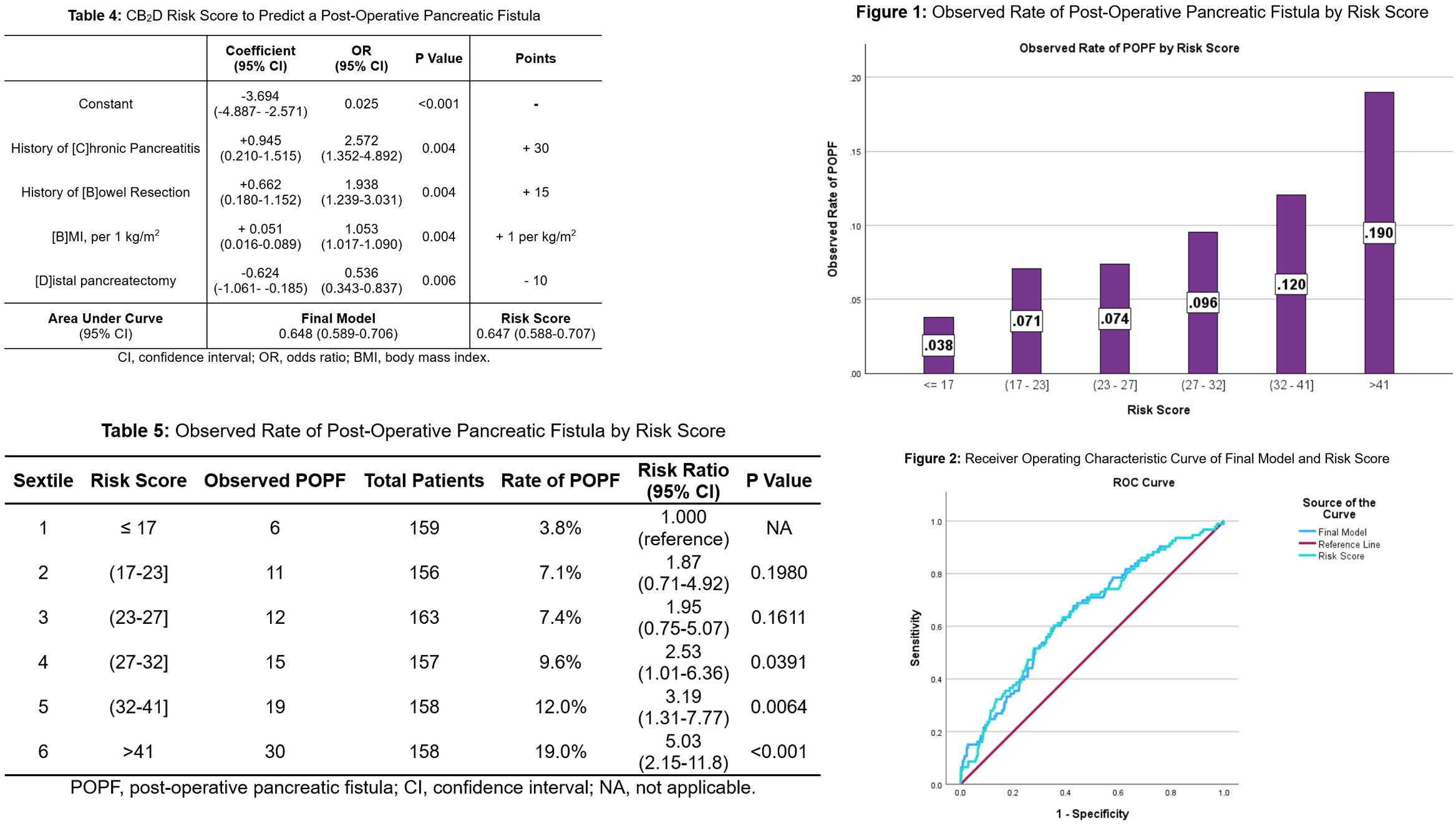
Figure 2: Derivation and Calibration Evaluation of Risk Score to Predict a Post-Operative Pancreatic Fistula