Background
Emergency pancreaticoduodenectomy (PD) is a complex surgical intervention with significant morbidity and mortality, and usually performed for traumatic indications. Studies suggest that up to 39.4% of non-traumatic cases are done for malignant causes including pancreatic cancer. We aimed to assess patient-level and hospital-level factors associated with emergency presentation for pancreatic cancer and the use of PD in emergency versus elective settings for pancreatic cancer.
Methods
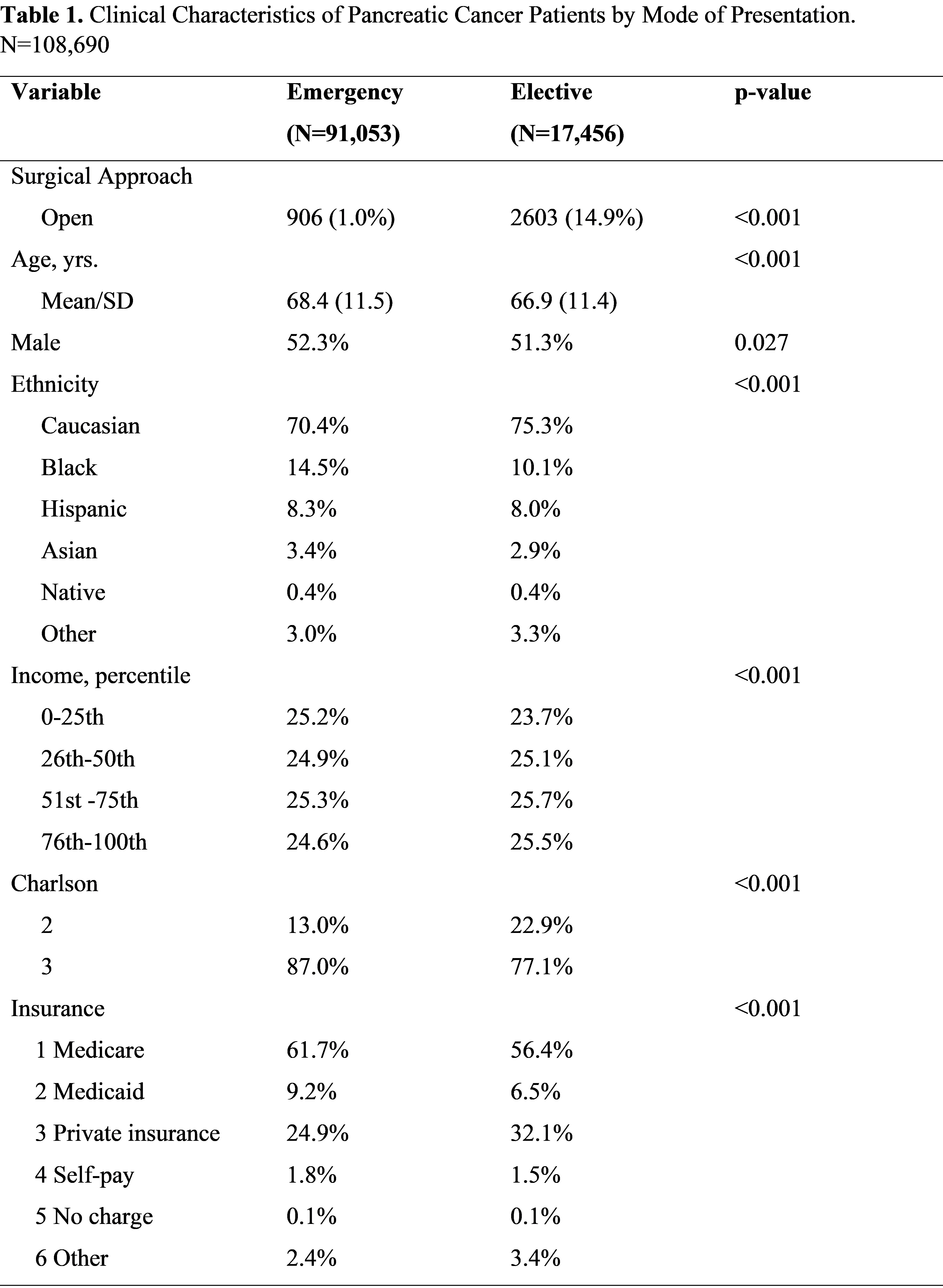
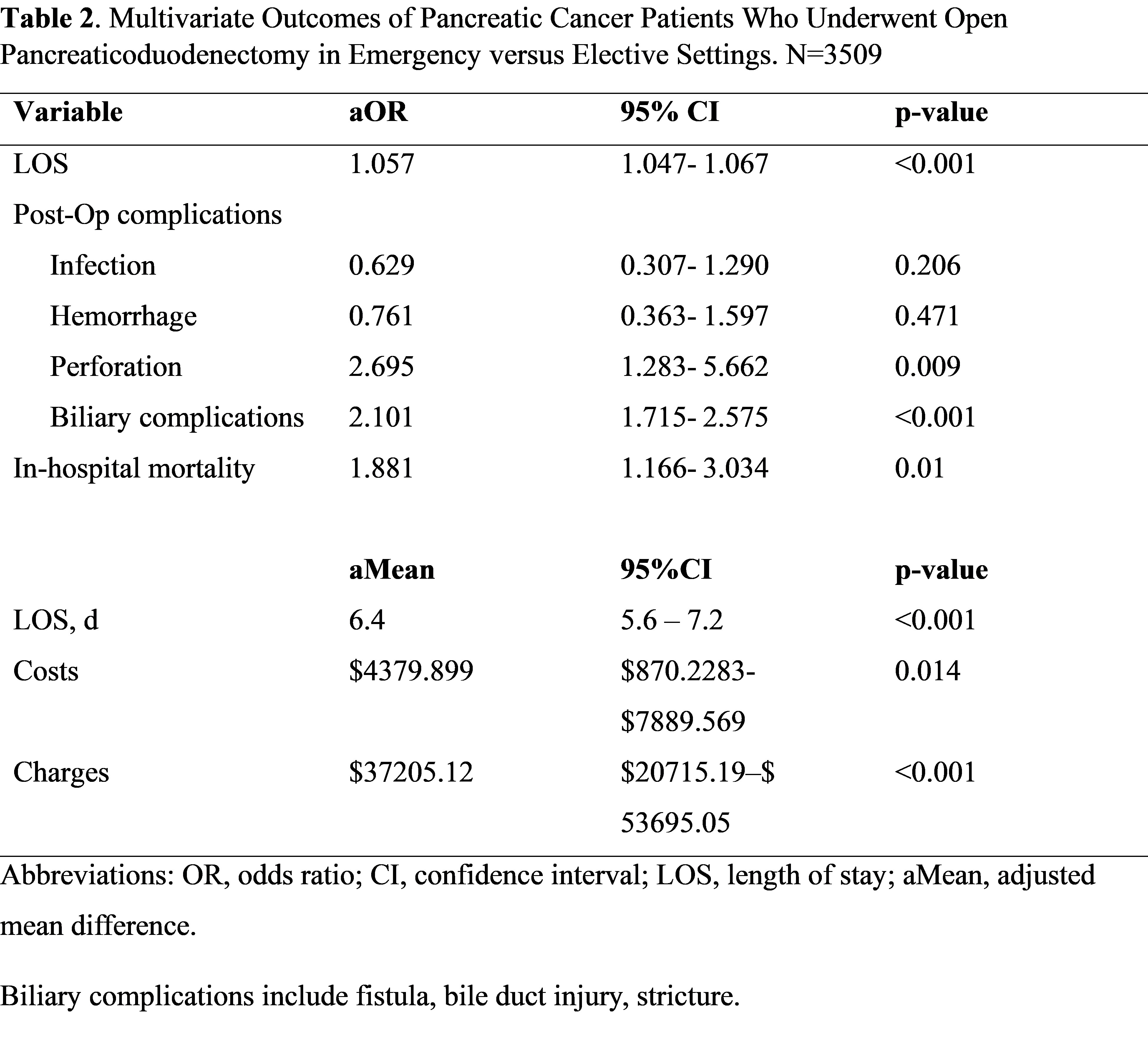
We examined the National Inpatient Sample (NIS) database from 2016-2020 to retrospectively identify pancreatic cancer admissions using ICD-10- CM codes. Patients who had open PD were included. Patients were stratified according to mode of presentation i.e emergent versus elective. Multivariable analyses were performed to assess differences in age, sex, ethnicity/race, income, insurance, Charlson Comorbidity Index (CCI), and hospital characteristics associated with mode of presentation. Surgical outcomes including length of stay (LOS), complications, expenditures, and in-hospital mortality were analyzed by mode of presentation.
Results
Of 108,690 pancreatic cancer patients identified, 91,053 (83.9%) were emergent admissions and 17,456 (16.1 %) were elective admissions. Emergency presentations were more likely to be Black (14.5% versus 10.1%), Medicare- (61.7% versus 56.4%) or Medicaid-insured (9.2% versus 6.5%), have 3 or more comorbidities (87.0%% versus 77.1%%), treated in small (16.6% versus 13.0%) or medium-sized (26.7 versus 21.4%) or urban nonteaching hospitals (17.4 versus 10.7%). Of 3509 patients who underwent open PD, 25.8% were emergency cases versus 74.2% elective cases. Predictors of Emergency PD include Black race, Medicaid, low income, small or medium-sized hospitals, and rural or urban nonteaching hospitals. Emergency PD cases displayed increased odds of perforation (aOR: 2.7, p =0.009), biliary complications (aOR: 2.1, p <0.001) and in-hospital mortality (aOR: 1.9, p =0.001). The adjusted additional mean hospital LOS, costs and charges were higher by 6.4 days, ,380 and ,205, respectively in the emergency cases.
Conclusion
Emergency pancreatic cancer presentations are associated with Black race, Medicare or Medicaid insurance, multiple comorbidities and nonteaching hospitals. Emergency pancreaticoduodenectomy was most likely in socially disadvantaged patient populations and associated with worse surgical outcomes.