Background: Evaluation of the quality of care delivered to patients with stage IV pancreatic adenocarcinoma (PDAC) has been limited. We sought to evaluate racial / ethnic disparities among patients treated for stage IV PDAC and the impact on outcomes using a novel and easily applied composite quality metric.
Methods: Medicare beneficiaries who were diagnosed with stage IV PDAC between 2004-2016 were identified using SEER-Medicare. Achievement of a quality score consisting of 3 individual criteria was assessed: (1) cancer-specific survival (CSS) > 12 months; (2) receipt of systemic therapy; (3) utilization of hospice / palliative care services. Factors associated with achieving quality score including race/ethnicity, social vulnerability index (SVI) and year of treatment were examined.
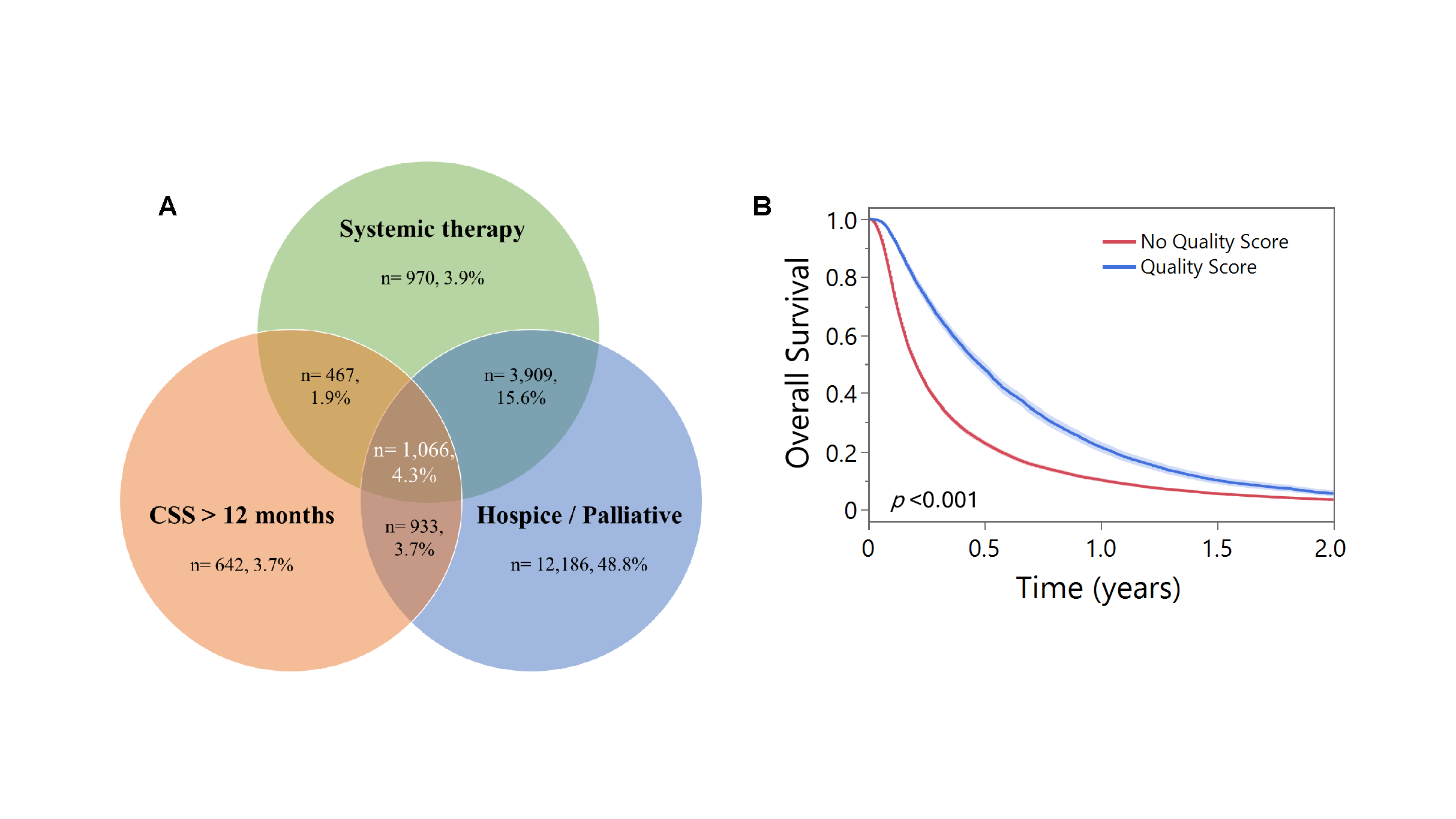
Results: Among 24,990 patients with stage IV PDAC, 18,094 individuals (72.4%) utilized hospice / palliative care services, 6,412 (25.7%) received systemic therapy, whereas 3,108 (12.4%) had CCS > 12 months after diagnosis. A total of 1,066 (4.3%) patients met all 3 individual criteria of the composite quality score (Figure 1A). Achievement of the composite quality score increased over time (2004-2007: 2.6% vs. 2008-2011: 4.5% vs. 2012-2016%: 5.4%, p<0.001). On multivariable analysis, racial / ethnic minorities (OR 0.71, 95%CI 0.60-0.85), as well as patients with higher SVI (ref low SVI; medium SVI: OR 0.83, 95%CI 0.71-0.97; high SVI: OR 0.76, 95%CI 0.65-0.89) were less likely to achieve the composite quality score after adjusting for other relevant covariates. Achievement of the composite quality score (excluding CSS criterion) was associated with improved OS (1-year OS: 21.4% vs 10.2%, p<0.001) (Figure 1B).
Conclusion: Roughly 1 in 25 patients with stage IV PDAC achieved the composite quality score with lower achievement among racial / ethnic minority patients and socially vulnerable populations. Lower achievement of the quality score was associated with worse long-term survival. These findings highlight the need to target interventions to achieve quality metrics among all patients with PDAC to mitigate disparities in end-of-life care.