Introduction
Spleen-preserving distal pancreatectomy is indicated for benign and low-grade malignant left-side pancreas lesions. There are two described approaches; Kimura -splenic vessel preserving distal pancreatectomy (SPVP-DP) where both the splenic artery and vein are preserved. As well as the Warshaw technique, where the splenic artery and veins are sacrificed with preservation of the short gastric vessels. Although the Warshaw technique is technically more feasible and less challenging, particularly for a minimally invasive (MI) approach, preservation rate of the spleen is lower than that of SPVP-DP. Furthermore, the significance of long-term complications, including sinistral hypertension is poorly understood. Conversely, SPVP-DP is usually indicated for smaller tumors and non-malignant cases and MI-SVP-DP is more complex and technically challenging. We propose a novel technique in which the splenic vein is preserved, to provide a more feasible yet successful approach to splenic preservation for patients with benign and low-grade malignant disease.
Method:
Our series includes five patients (3 male and 2 female, age 52 who underwent SPVP-DP at the Austin Hospital and Warringal Private Hospital, Victoria, Australia between November 2022 and July 2023. SPVP-DP was performed for 1 mucinous cystic neoplasm, 1 IPMN with worrisome features, 1 with abnormal lesion with BRCA 2 mutation, 1 for chronic pancreatitis and 1 serous cystadenoma. Three patients underwent an open approach, and two patients with MI approach including one laparoscopic approach, and one robotic approach with Da Vinci Xi.
Our technique involved ligations of the splenic artery (SpA) with preservation of the splenic vein and short gastrics. (Operative video will be presented). At the end of the operation, we performed an indocyanine green (ICG) angiogram and venogram to confirm spleen viability and splenic vein anterograde flow (Figure 1).
Results
Postoperatively, there was one case with Grade B pancreatic fistula. No splenic infarction nor gastric varices are observed in follow-up cross-sectional imaging at 3 and 6 months postoperatively. One patient developed limited splenic vein thrombosis with a normal appearance of the spleen.
Conclusion
Splenic vein preservation might be fundamentally more important than that of splenic artery for the preservation of the spleen. Maintaining adequate outflow for solid organ might underestimated. We have limited data with a small study group available; therefore, more long-term follow-up and multicentre trials are warranted.
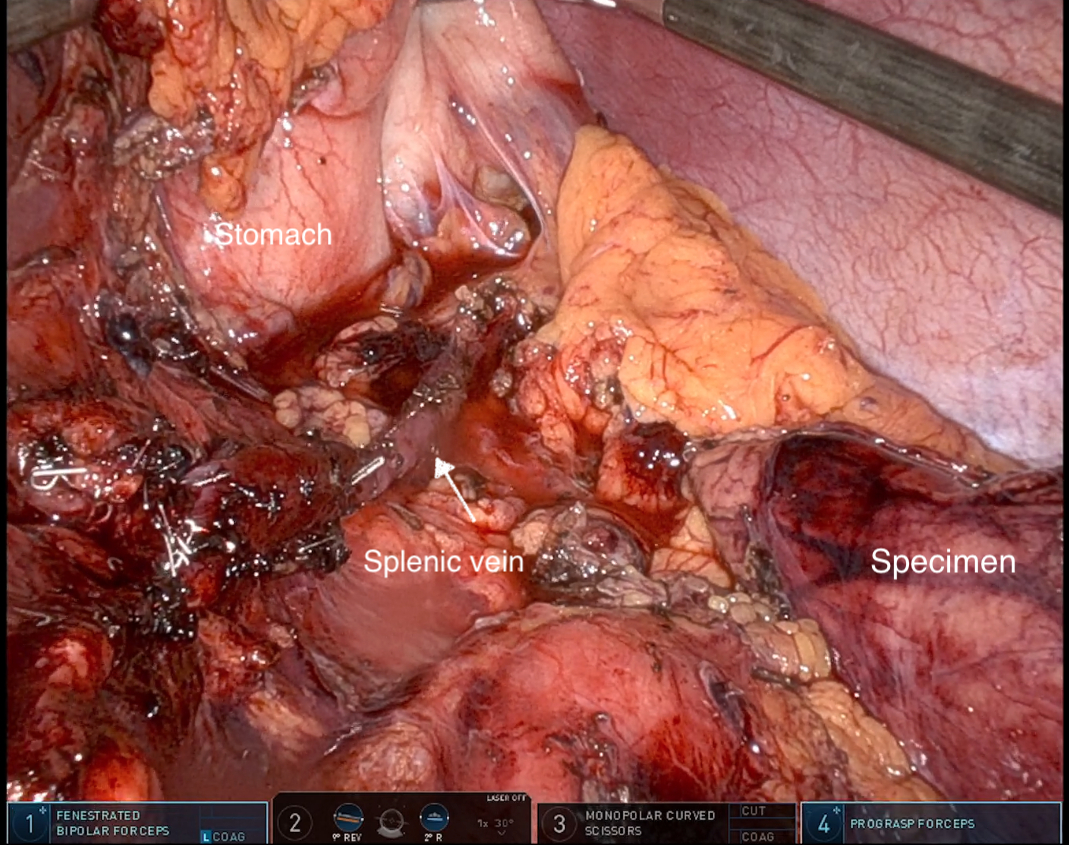
Figure 1a. Intraoperative picture after the resection. The splenic vein was dissected but remained intact. It is of note that the splenic artery was ligated twice at the proximal and distal end.

Figure 1b. Intraoperative ICG angiogram and venogram demonstrating anterograde venous flow in splenic vein.