Background Esophageal squamous cell carcinoma (ESCC) and Adenocarcinoma (EAC) are the two most common histological types of esophageal cancer (EC) worldwide. Although both belong to EC, risk factors, tumor locations and surgeries vary between EAC and ESCC. Geographically, Shanxi Changzhi in mid-north China has a substantially high EC incidence, yet limited patient data were reported given underdevelopment. This research aims to investigate the patient demographics and surgical care of EAC and ESCC in a regional Shanxi Changzhi hospital.
Method Patient charts, surgical notes, and pathology reports were extracted from May to July 2023 for hospitalized EC patients. Patient age, gender, primary and secondary diagnoses, pathology, surgical treatment, and length of stay (LoS) were recorded. A random sample of surgical cases in July was observed to validate the surgical operation notes.
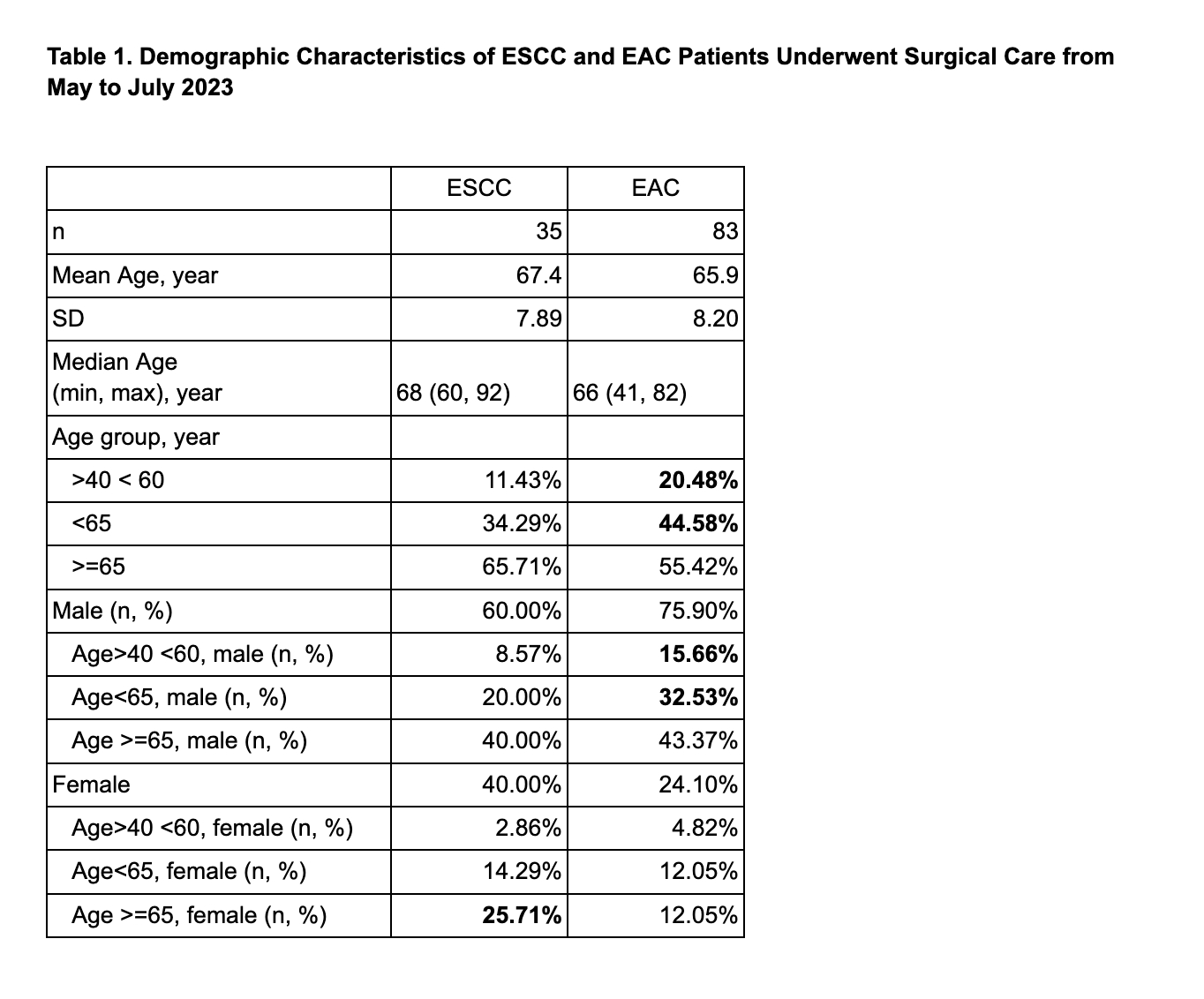
Results A total of 35 ESCC and 83 EAC patients were admitted to surgical units of the hospital in the 3-month timeframe. All 83 (100%) EAC patients were admitted in Gastrology, 33 (94.3%) ESCC patients in Thoracic, and 2 (5.7%) in Gastrology.
EAC has higher occurrences in males than ESCC (75.9% vs. 60.0%). Although median and mean ages were similar (EAC: median age=66 and mean age=65.98.2; ESCC: median age=68 and mean age=67.47.89), EAC patients have a higher proportion of young age groups (EAC: 20.48% in age> 40 <60; ESCC: 11.43% in age >40 <60).
Tumor locations were at esophagogastric junction in 81 (97.6%) of the EAC patients, in esophageal in 33 (94.3%) ESCC patients, and at esophagogastric junction of the 2 (5.7%) ESCC patients admitted to Gastrology department. Among patients with confirmed TNM staging, the majority of them were in T3 or T4 stages with M0.
Surgical care for ESCC patients in thoracic included chemotherapy infusion, thoracoscopic three-incision esophagectomy, or combined thoraco-laparoscopic three-incision radical esophagectomy (with or without closed chest drainage); none of the 33 patients underwent open thoracic surgery. For EAC and ESCC patients admitted to Gastrology, surgical care included chemo- or other therapy infusion, laparoscopic radical proximal or total gastrectomy, or open radical proximal or total gastrectomy. Hospital LoS was associated with the type of surgical care.
Conclusion EAC was disproportionately higher in younger age groups and in males than ESCC in Shanxi Changzhi. Different tumor locations of ESCC and EAC resulted in different department admissions and different surgical care. The research sheds light on separating ESCC and EAC in EC reporting, calling for further patient surveys investigating lifestyle risk factors and coordination of care for EAC and ESCC patients in this highly prevalent, underdevelopment region.