Objective: Endoscopic submucosal dissection (ESD) of esophageal tumors remains controversial in the West despite wide use internationally. Endoscopic mucosal resection (EMR) is more widely deployed as a result of its relative technical ease, more reliable reimbursement, and lower morbidity—prominently, lesser incidence of stricture formation. Our goal is to evaluate factors associated with stricture formation in ESD from a single Western center.
Methods: We retrospectively reviewed our institutional prospective quality database for all patients who underwent ESD for esophageal lesions both benign and malignant from 2020-2023. Our practice changed over time to include variable stricture prophylaxis. Modalities deployed include PPI, oral sucralfate, and spray topical steroids intra-op. Procedure data and outcomes, as well as patient-reported quality of life using Functional Assessment of Cancer Therapy-Esophagus (FACT-E) were recorded.
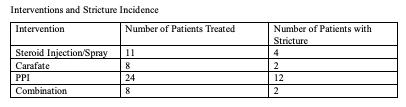
Results: 26 patients (age 50-81; 89% male; 77% Caucasian, 23% African American; mean BMI 26.4) underwent ESD for early esophageal neoplasia (5 BE-HGD, 5 pT1a, 9 pT1b, 3 pT2, 4 other). Overall mean resection circumference was 58.5% (range 33-80), mean pathologic size of lesion 25.4 mm (20-35), and mean area of resection 28.2 mm (12-48). Patients were followed post operatively for an average of 16 months. Overall post-ESD stricture formation rate was 50% (13 of 26) with similar rates of 42% for invasive cancer (T1b, T2) and 57% for all other indications (RR 0.73, 95% CI 0.32-1.64, P .44). Most required 1 dilation (range 1-20, mean 3). Size of lesion, circumferential extent and total area resected, and patient BMI were not independently associated with stricture formation. Stricture prophylaxis with steroid injection/spray (odds ratio 0.381; 95% CI 0.077, 1.89; P .214), oral sucralfate (OR 0.21; 95% CI 0.033, 1.36; P .101), and in combination (OR 0.63; 95%CI 0.258, 1.571, P .26) did not reach significance but trended toward decreasing stricture incidence. There was no association between PPI use and stricture development. Complications other than stricture occurred in 4 patients (1 atrial fibrillation, 2 bleeding, 1 perforation after stricture dilation managed with antibiotics). When asked if they would undergo ESD again, all respondents (18 of 26 total patients) said yes.
Conclusion: ESD is associated with high patient satisfaction despite the risk of stricture formation and should be considered a safe alternative to esophagectomy in patients with a wider range of esophageal pathology including benign disease and early invasive cancer.