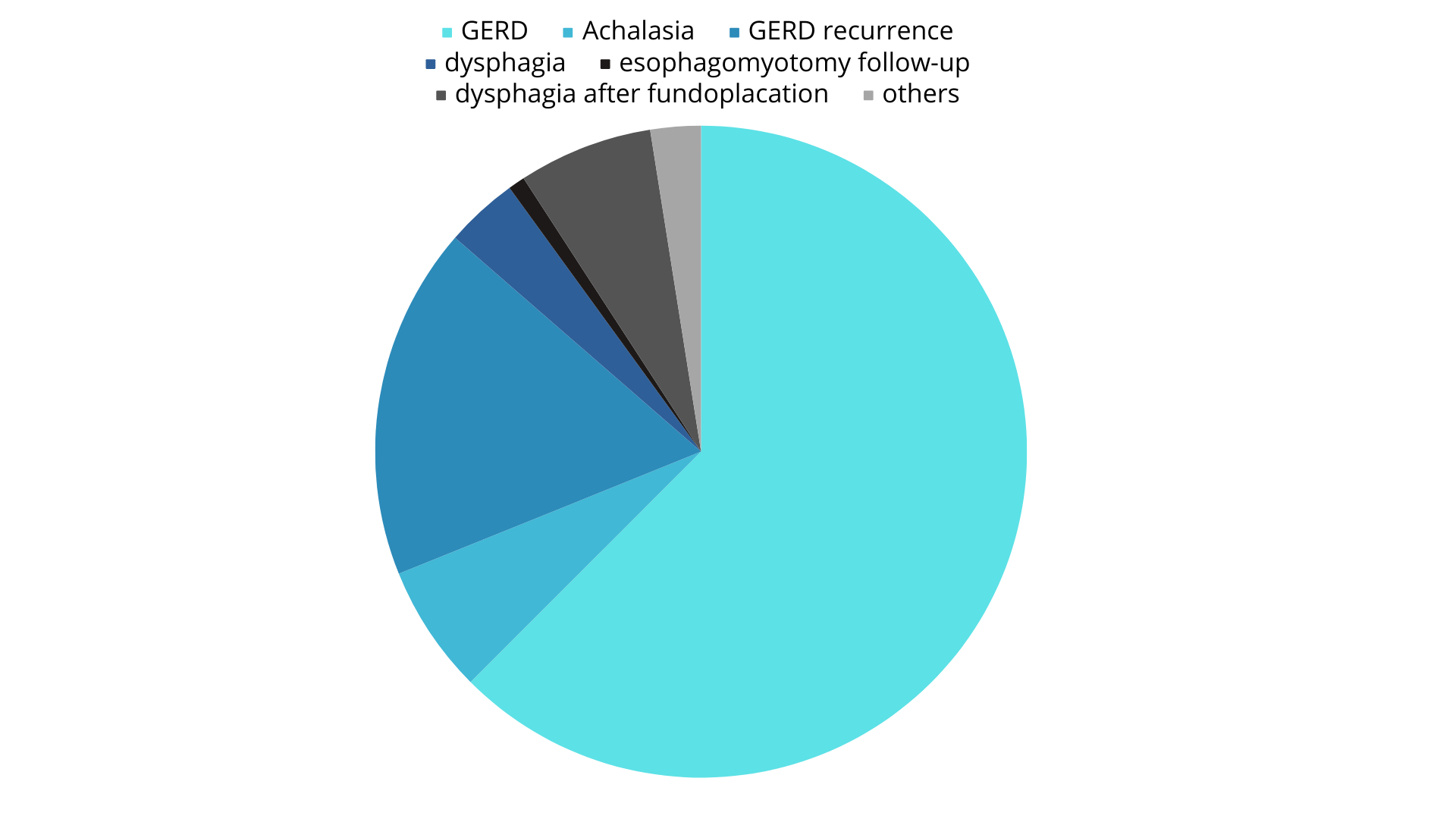
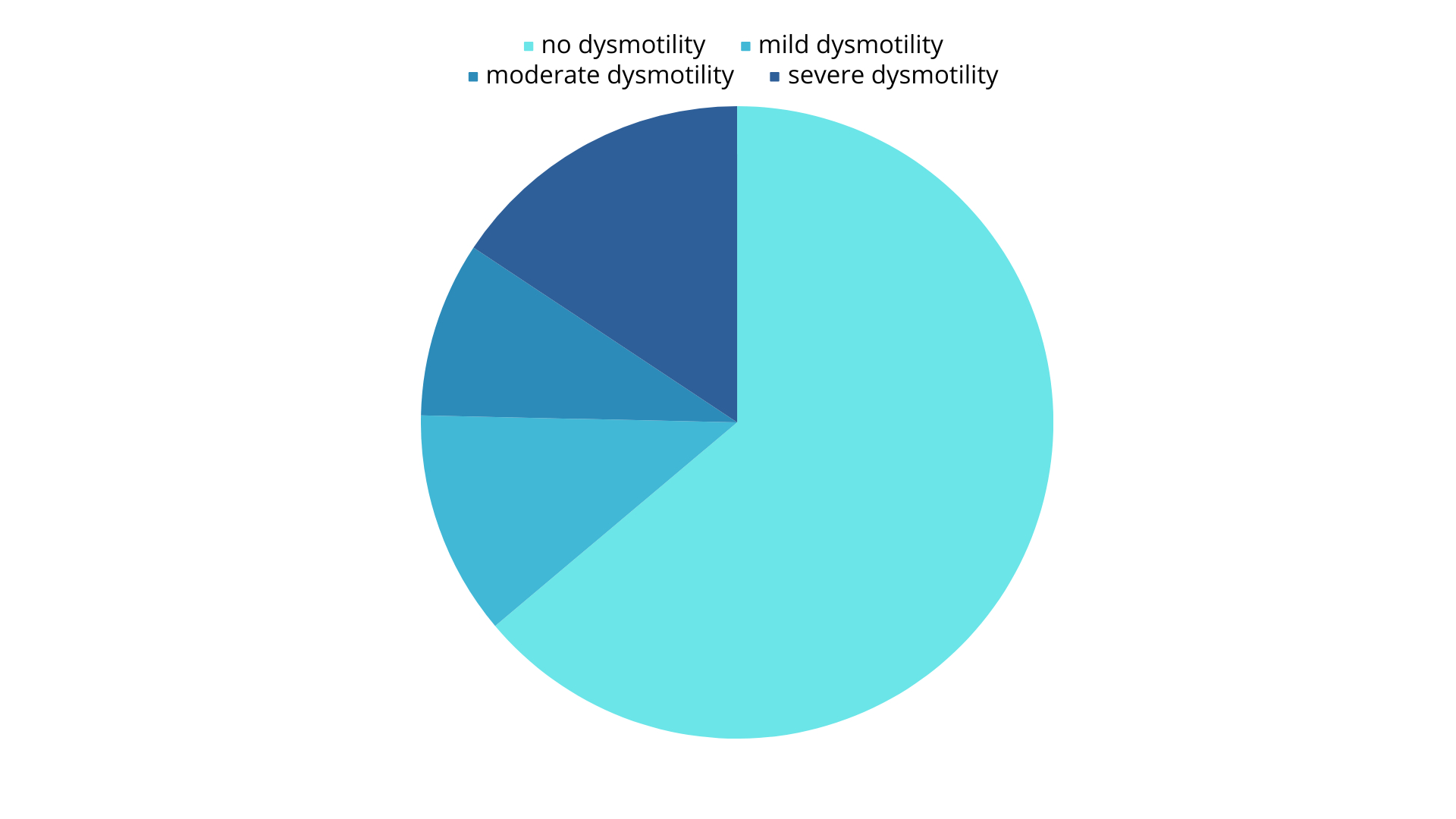
INTRODUCTION: Among disorders of the upper gastrointestinal tract, esophageal motility disorders stand out due to their high prevalence and morbidity. In this sense, the present work aims to report the experience of the Motility Lab of Foregut Unit in Digestive Surgery Service of the Hospital de Clínicas de Porto Alegre, Rio Grande do Sul, Brazil, in monitoring patients who underwent esophageal electromanometry studies, mainly before surgery indication, in the last 6 years. METHODS: From January 2017 to June 2023, 358 exams were carried out to evaluate esophageal motility. It was a prospective databank which we review retrospectively all the exams performed. RESULTS: Our population was predominantly female (76%) and with an average age of 57.4 years (16 - 86 years). The individual indications for carrying out the exam are found in table 1. Among the results, 228 (63.68%) patients did not present any level of dysmotility, 73 (20.39%) presented mild or moderate dysmotility, and 56 (15.64%) resulted in marked dysmotility (table 2). In 212 cases, Impedanciometry was used, which confirmed insufficient progression (<70%) of food bolus in 152 individuals. The anatomy of the esophageal hiatus of the diaphragm, through X-ray examination with oral contrast, was also evaluated in 323 of these patients, of which 51% had the presence of a diaphragmatic hiatal hernia confirmed. The exams were carried out to evaluate anatomical and morphological changes in the lower esophageal sphincter as well as the prevalence of motor disorders in these patients. Registration was made in the unit's own database along with symptom assessment for subsequent epidemiological analysis. DISCUSSION AND CONCLUSIONS: Esophageal motility disorders are prevalent among patients with GERD symptoms and other surgical conditions of the upper GI tract, including an esophageal motility study prior to surgical evaluation must provent key informations of the esophagogastric junction outflow and about peristaltic disorders. Patients with abnormal motility more likely report esophageal symptoms. Care should be taken in these particular patients to avoid a wrong surgical indication if there is one. Our population has a uniform pattern of IEM, with a minority of cases with a severe dismotility.