Background: Endoscopic resection techniques have emerged as an alternative for treating early stage esophageal cancer but come with a steep learning curve, uncertain reimbursement, and controversial long-term outcomes. We evaluated a single surgeon experience for technical success, complications, and lesion sizes. We also queried post-operative quality of life comparing ESD to a stage-matched esophagectomy group.
Methods: Retrospective review was conducted following IRB approval of a prospective quality database at our institution from 2020-2023. Patient records were reviewed to investigate past medical history, final pathology and resection margins, hospital course, and outcomes. Patient-reported impacts on quality of life were obtained with Functional Assessment of Cancer Therapy-Esophagus (FACT-E).
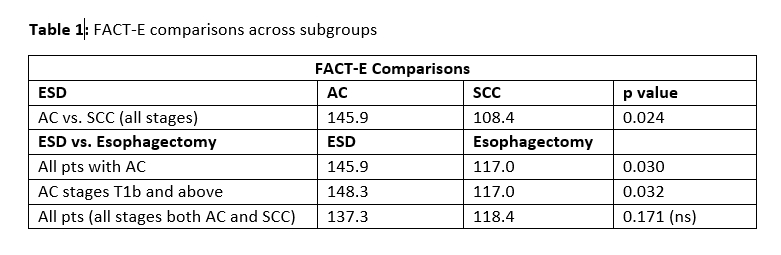
Results: Twenty-six total patients (age 50-81; 88% male; 82% Caucasian, 18% African American) underwent ESD, 21 for early esophageal cancer or Barrrett esophagus with high-grade dysplasia (BE-HGD) (14 adenocarcinomas [AC] - 5 T1a, 7 T1b, 2 T2; 3 squamous cell carcinomas [SCC] - 2 T1b, 1 T2). Technical success was achieved in 100% and all were discharged home same day. Complications include: 2 patients with late bleeding (> 48 hrs),1 patient with late perforation (> 48 hrs), and 8 patients who developed strictures, managed most often with 1 dilation session (range 1-20). At a median follow-up of 13 months (1-32 months), only 1 patient (3.85%) had local cancer recurrence (AC). This patient had received adjuvant therapy with cryoablation and yearly surveillance EGDs. There were 7 of 17 invasive cancers that had an R1 resection with 1 positive lateral margin who underwent ablation and 6 positive deep margins. The deep R1 group were entirely T2 or deep T1b disease patients. Recurrence was not impacted significantly by margin (R0 vs R1), size of lesion, or adjuvant therapy. All 13 who responded to surveys (100%) reported they would undergo ESD again. Thirteen patients (age 51-75; 85% male; 85% Caucasian, 15% African American) who had undergone esophagectomy for early esophageal cancer (11 AC - 5 T1b, 6 T2; 2 SCC - 1 T1a, 1 T2) were identified. The average hospital length of stay (LOS) was 23.4 days. 4 patients (30.7%, 3 AC, 1 SCC) experienced recurrence of disease, 1 resulting in death. Patients with AC of all stages who underwent ESD reported a better quality of life than those who underwent esophagectomy (Table 1: FACT-E of 146 vs. 117, p = 0.03).
Conclusions: ESD was achievable with acceptable R0 and complication rates and improved patient satisfaction. Long-term survival outcomes will help clarify its role in managing a complex disease.