Background
Laparoscopic Nissen-Rossetti fundoplication (LNRF) is a highly effective tratement for gastroesophageal reflux disease (GERD), based on objective evidence of reflux as the cause of ongoing symptoms. LNRF is a variation in the surgical technique where the short vessels are not ligated. This results in a shorter surgical time and less manipulation of structures. Over time, there has been ongoing discussion regarding whether this approach is the superior treatment compared to the conventional technique. True failures after antireflux surgery are uncommon, typically occurring within the first 2 years. Patients considering surgery are concerned about adequate control of reflux symptoms and the risk of adverse outcomes, including persistent troublesome side effects. Long-term follow-up scales, assessing symptoms like acid regurgitation, dyspepsia, dysphagia, and gas-bloat syndrome, have been designed. The aim of this study is to evaluate the quality of life in patients who underwent Laparoscopic Nissen-Rossetti fundoplication after 5 or more years of surgical intervention.
Materials and Methods
A long-term, single-center, retrospective study of 16 laparoscopic fundoplication with a minimum of 76 months follow-up. The patients were asked to complete the GERD-HRQL questionnaire, and the Visick scoring system was applied. Additionally, the patient's weight and the use of PPIs pre and postoperatively were compared. All surgeries were performed by the same surgeon using the same surgical technique. Statistical analysis was performed using STATA Software v13 and a p-value < 0.05 was considered the statistical significance level. Student’s or Mann–Whitney U tests were used to evaluate differences between the two groups.
Results
Sixteen patients (11 females, 5 males) underwent laparoscopic Nissen-Rossetti fundoplication (LNRF) with 67% undergoing the procedure for gastroesophageal reflux disease (GERD). Follow-up spanned 76 months post-intervention, during which 83% ceased proton pump inhibitor (PPI) use even for 6 years after the intervention. BMI showed no significant variance (26.9 vs. 24.6, p=0.61). Postoperative GERD-HRQL scores revealed no significant differences between those discontinuing PPIs and those continuing (14.5 vs. 5.5–13, p=0.28). Similar non-significant trends were observed in VISICK scores (2.5 vs. 1.5, p=0.68).
Conclusion
LNRF is the preferred method for GERD. Despite the rise of endoscopic procedures, laparoscopy remains cost-effective, especially in resource-limited settings. Evaluating patient satisfaction and quality of life emerges as crucial post-surgery, especially in clinical practice and in-depth studies focusing on longer-term follow-up outcomes. To improve study validity, larger-scale research with an extended follow-up is needed.
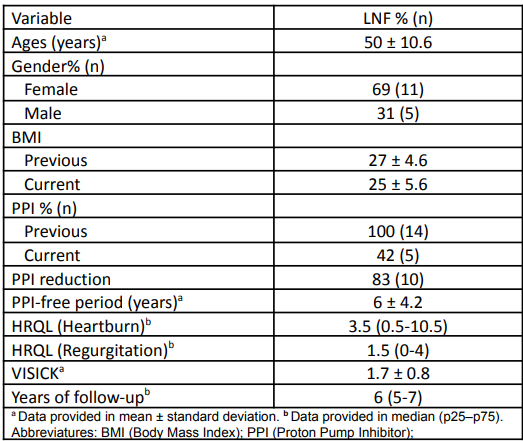
Characteristics of patients who underwent laparoscopic Nissen-Rossetti Fundoplication (LNF).
Postoperative scale scores for the assessment of quality of life and patient satisfaction