Introduction
The 5-year survival of patients diagnosed with esophageal adenocarcinoma (EAC) in the United States has improved 4x from less than 5% in 1975 to more than 20% in 2015. Neoadjuvant chemoradiation (NCRT) has been instrumental in improving patient survival as it reduces tumor size and stage prior to surgery. However, not all patients receive similar benefit from NCRT. The aim of our study is to assess which demographic and clinical characteristics are associated with downstaging following receipt of NCRT.
Method
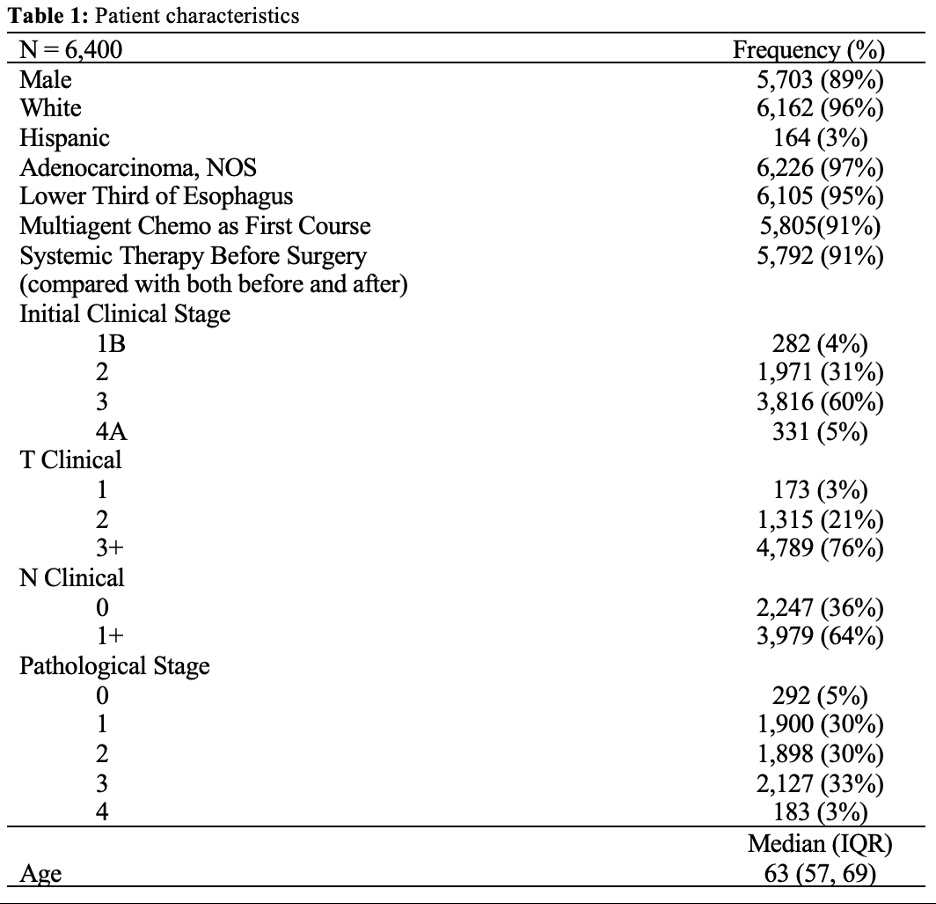
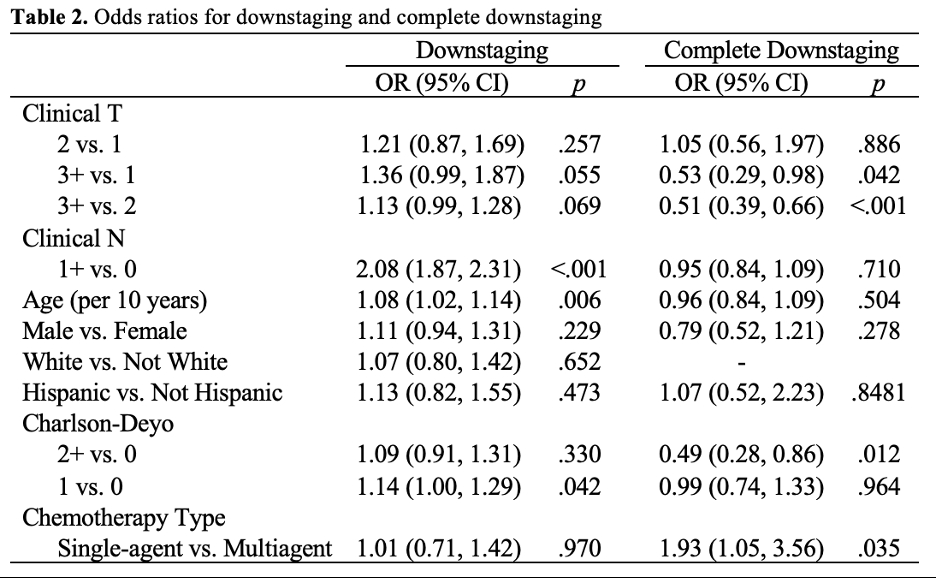
Using the 2010-2020 National Cancer Database, we identified 6,400 patients with EAC who received NCRT. Multivariable logistic models were estimated to evaluate odds of downstaging, with downstaging defined as a lower pathological stage compared to pre-NCRT clinical stage and complete downstaging defined as pathologic stage 0 (i.e., pT0N0). Covariates included age at diagnosis, biological sex, race, ethnicity, Charlson-Deyo score, as well as type of chemotherapy delivered (single agent vs. multiagent) and clinical T and N category.
Results
The patient sample primarily consisted of older white males receiving multiagent chemotherapy (Table 1). In total 3,285 (51%) patients experienced any downstaging, with 292 (5%) completely downstage – both as defined above.
Higher Clinical N stage was associated with 108% higher likelihood of any downstaging (OR: 2.08, 95% CI: 1.87- 2.31, p <.001), but 5% (non-significant) lower likelihood of complete downstaging (OR 0.95, 95% CI: 0.84 - 1.09, p = .710) (Table 2). Similarly, higher clinical T, for example clinical T of 3+ compared with 1, was associated with an estimated though non-significant 36% higher likelihood of any downstaging (OR: 1.36, 95% CI: 0.99 - 1.87, p = .055), but a 47% lower likelihood of complete downstaging (OR: 0.53, 95% CI: 0.29 – 0.98, p = .042). Further, when compared with a Charlson-Deyo score of 0, a score of 1 resulted in a 14% higher likelihood of any downstaging (OR: 1.14, 95% CI: 1.00 - 1.29, p = 0.042), while a score of 2+ resulted in a 51% decreased likelihood of complete downstaging (OR: 0.49, 95% CI: 0.28 – 0.86, p = .012).
Discussion
Our study showed that, EAC patients with clinically diagnosed lymphatic involvement who underwent neoadjuvant chemoradiation, were more than twice as likely to achieve tumor downstaging compared to patients with no lymph node involvement. Patients with T3+ EAC were almost half as likely as patients with T2 or T1 EAC to achieve complete downstaging following neoadjuvant chemotherapy. While downstaging has been shown to be associated with increased survival, more research is needed to fully understand the effects of downstaging as it pertains to stage specific, patient prognosis.