Objective: Endoscopic peroral plication of the esophagus (POPE) is a novel alternative to esophagectomy for the treatment of megaesophagus that develops in end-stage achalasia. Early reports have shown promising results with POPE providing subjective symptom relief and visual improvement on barium esophagram. Our goal is to further determine if POPE is an effective treatment for megaesophagus and to explore objective measures of outcomes, including timed barium esophagram (TBE), Eckardt Score, GERD-Health Related Quality of Life (GERD-HRQL) Questionnaire, and Reflux Symptom Index (RSI) to help predict success.
Methods: Retrospective review was performed on a prospectively maintained database of patients with achalasia, symptomatic megaesophagus, and pre-op balloon distensibility confirming interrupted lower esophageal sphincter who underwent POPE at our institution in 2023. All patients completed pre-and post-operative timed barium esophagram, Eckardt Score, GERD-HRQL, and RSI as per our standard of care.
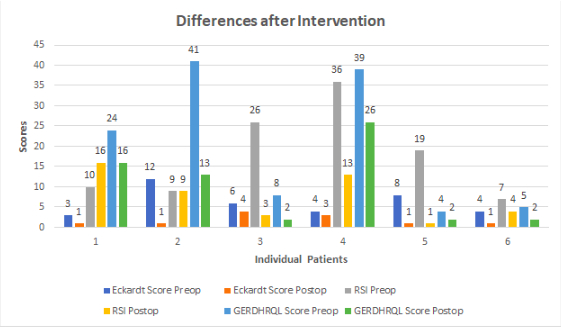
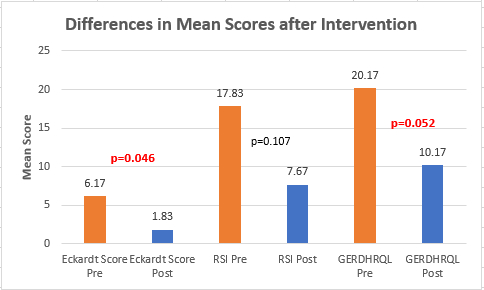
Results: 6 patients (age > 18; 50% Caucasian, 50% African American; 66.6% female; mean BMI 29.11) underwent POPE with an average 3.33 (range 2-7) sutures used per patient and mean operative time of 96.8 (range 77-152) minutes. Midterm follow-up data (6-12 weeks) was available on all 6. Mean total Eckardt score decreased from 6.17 pre-operatively to 1.83 post-operatively with an average decrease of 3 points per patient (p-0.046; CI = 0.88 - 5.912). Symptom subscales further revealed significant decreases in dysphagia (0.833; p-0.046; CI = -0.198 – 1.865), regurgitation (1.167; p-0.058; CI = -0.060 – 2.394), and chest pain (1.333; p-0.025; CI = 0.249 – 2.417) independently. GERD-HRQL also demonstrated significant post op symptom improvement with an average 10 point decrease in total score (p-0.052;CI= -0.131 – 20.131). RSI showed an overall 10.16 point decrease in total score but did not reach statistical significance (p-0.107; CI - 3.164 – 23.498). Interestingly, TBE comparison revealed a 3.67 cm increase in max transverse diameter (p<0.001; CI = -1.22 - 0.495) despite visual improvement in sump formation and esophageal diameter, which may be attributable to variation in radiologist site of measurement. One bleeding complication occurred requiring repeat endoscopy without transfusion or further incident.
Conclusion: This is the 3rd largest case series of patients undergoing POPE for megaesophagus in the United States. Our results support previous studies that POPE is safe and effective and demonstrate that patient reported outcomes (Eckardt score and GERD-HRQL) correlate with significant symptomatic improvement. Further standardization is required to determine the usefulness of TBE for POPE.