BACKGROUND: Esophagectomy is part of standard treatment for esophageal cancer. In recent years, hRAMIE has gained prominence among operative approaches. Complications of postoperative anastomotic strictures have been well described and persist in patients undergoing the robotic approach.
OBJECTIVE: This study evaluates the differences in clinical and enhanced recovery after surgery (ERAS) elements impacting development of anastomotic stricture following hRAMIE. We analyzed and summarized patient characteristics and inpatient ERAS benchmarks in patients who developed postoperative stricture requiring endoscopic interventions.
METHODS: Patient demographics, perioperative events, ERAS benchmarks, and the incidence of postoperative anastomotic leak and strictures in consecutive patient undergoing hRAMIE with circular stapled (EEA) esophagogastrostomy were collected prospectively and analyzed retrospectively from 2018 to 2023 at our institution.
RESULTS: A total of 105 consecutive hRAMIE patients were included and stricture vs non-stricture groups were compared. Average length of stay was six days with post-operative anastomotic leak rate of 11%. Thirty-eight (36%) developed postoperative strictures. There were no differences in patient characteristics (age, gender, cancer stage, comorbidities). There were also no differences in etiology, cancer progression, preoperative nutritional status, operative time, blood loss, or presence of anastomotic leak. However, patients who developed strictures had significantly more hypotensive episodes (sustained mean arterial pressure (MAP) < 70 mmHg) for more than 20 minutes during inpatient recovery (p<0.05). Multivariate analysis also revealed an odds ratio of 6.26 (95% CI: [2.06, 19], p<0.05).
No significant difference was observed in ERAS benchmarks.
The median time from surgery to the appearance of stricture symptoms was 51.5 days (8-488 days). These patients required a median of 4 (1-15) endoscopic interventional treatments, significantly more than in the non-stricture group (p<0.05).
CONCLUSION: Anastomotic strictures following hRAMIE occur two months postoperatively and increases the burden of endoscopic interventions during outpatient recovery. Inpatient hypotensive episodes appear to contribute to development of anastomotic strictures after hRAMIE. This study emphasizes the importance of inpatient normotension despite no differences in ERAS achievements in this cohort.
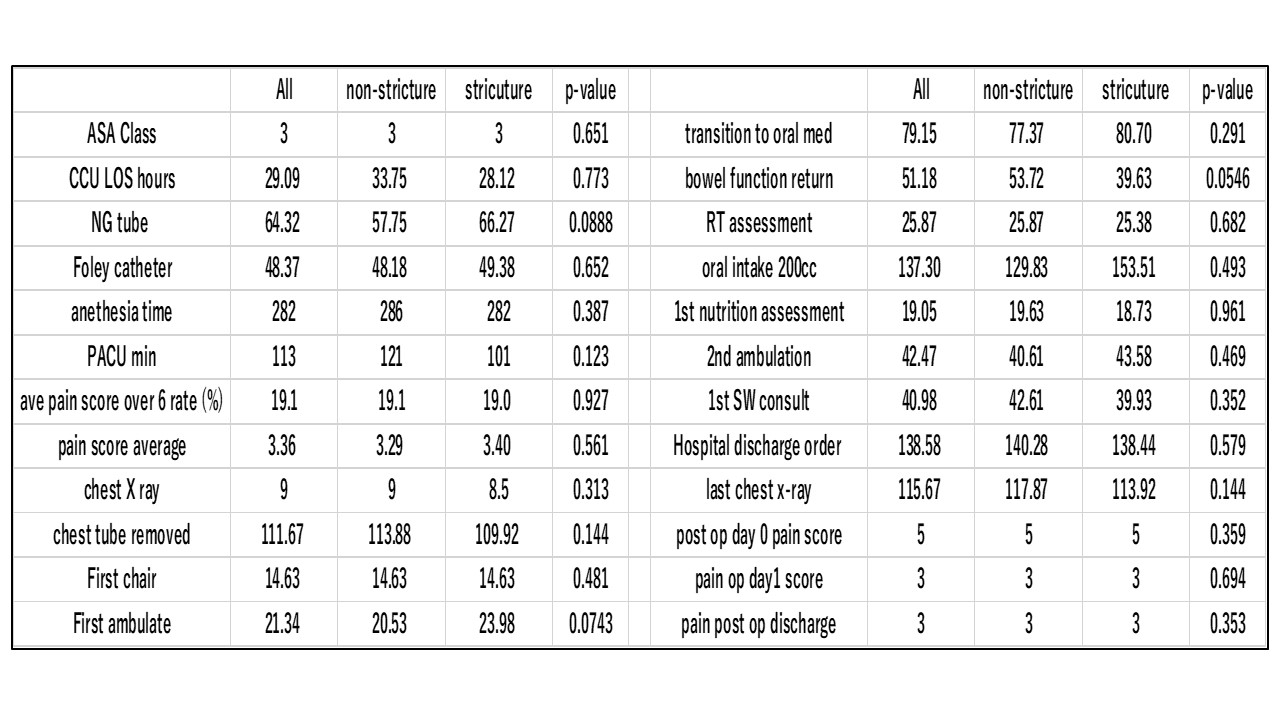
ERAS benchmarks