Introduction: The majority of comparative studies evaluating robotic and laparoscopic colorectal resections focus on immediate postoperative and clinical outcomes while lifestyle changes after discharge remain largely unstudied. Thus, we aimed to study postoperative recovery differences, specifically time to return to work, pain after discharge, opioid requirements at home, and activity levels, in patients who underwent colorectal resections by the robotic versus laparoscopic approach.
Methods: This is a retrospective study of patients who underwent robotic versus laparoscopic colectomies in our health system from 2020-2022. A validated survey was utilized to obtain responses. The primary outcome was time to return to work after discharge. The secondary outcome was postoperative pain after discharge, pain medication requirements at home, and activity level tolerance. Categorical variables were compared utilizing chi-square test. Continuous variables were compared by two-sided two sample t-tests. Mantel Haenzel test of trend was used for ranked variables. A p-value less than 0.05 was considered clinically significant.
Results: In total, 531 individuals were contacted of which 61 patients consented to participation in the laparoscopic (L) arm and 67 patients in the robotic (R) arm, corresponding to a 24% responder rate. The laparoscopic group had a higher proportion of patients with inflammatory bowel disease (IBD) (L 49% vs R 1%, P<0.0001), ostomy formation (L 30% vs R 15%, P=0.04), and intraoperative drain placement (L 53% vs R 31%, P<0.001). There was no difference in length of stay, or adverse events between the two groups. Both groups reported comparable readiness to go home and appropriate pain control on the day of discharge (Table 1). While a greater proportion of patients were working preoperatively in the laparoscopic group (L 61% vs R 36%, P=0.005), there was no difference in the number of patients who returned to work (L 73% vs R 78%, P=0.64), with a trend for earlier return to work in the robotic arm (L 3.8 weeks vs. R 2.3 weeks, P=0.09). Patients in the robotic arm noted overall reduced pain levels at home, with 73% of patient reporting no pain to mild pain 1 week after discharge (P=0.0013) (Figure 1). No difference was detected between the groups for opioid medication requirements at home (P=0.8) nor in the ability to tolerate light or moderate activity one week after discharge (P=0.3, P=0.11 respectively).
Conclusions
Patients who underwent robotic colectomies had reduced pain levels at home upon discharge, and demonstrated a trend for earlier return to work than patients who underwent laparoscopic colectomies. Postoperative quality of life, specifically return to work and functional status after discharge, are important metrics when determining surgical success and requires evaluation in larger studies.
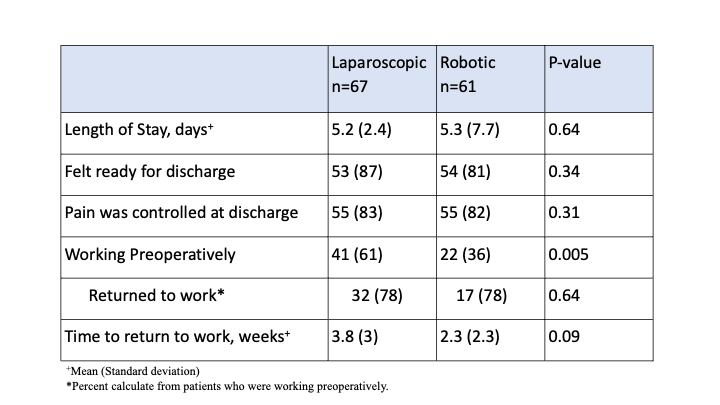
Table 1: Postoperative outcomes.
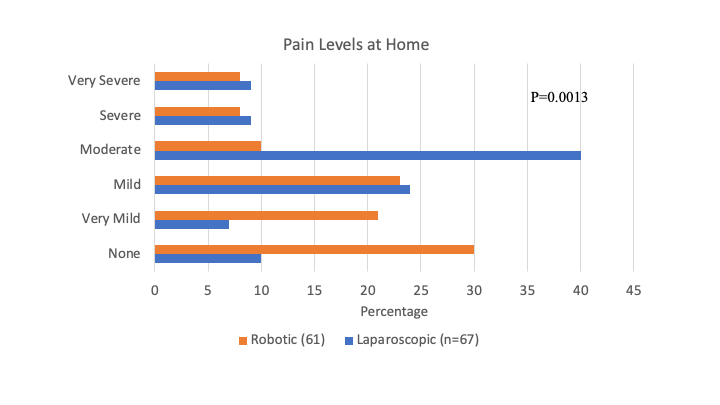
Figure 1: Pain levels 1 week after discharge.