Purpose
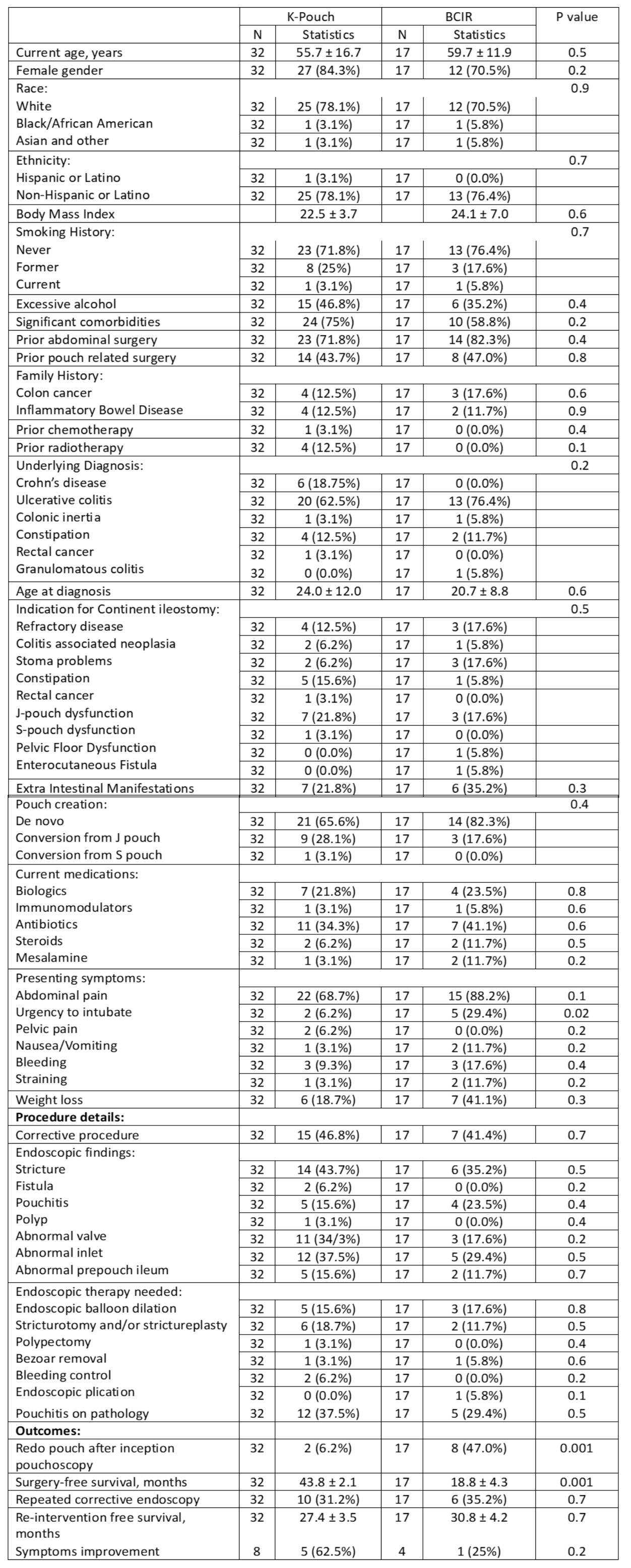
Continent ileostomy (CI) is a viable option for selected patients as an alternative to end-ileostomy or an ileoanal pouch after colectomy for ulcerative colitis or familial adenomatosis. CI consists of two forms, the Kock pouch and the less commonly performed Barnett Continent Intestinal Reservoir (BCIR). A comparison of outcomes of the two configurations of CI has not been reported in the literature. This study aims to compare the clinical outcomes of two configurations of CI.
Methods
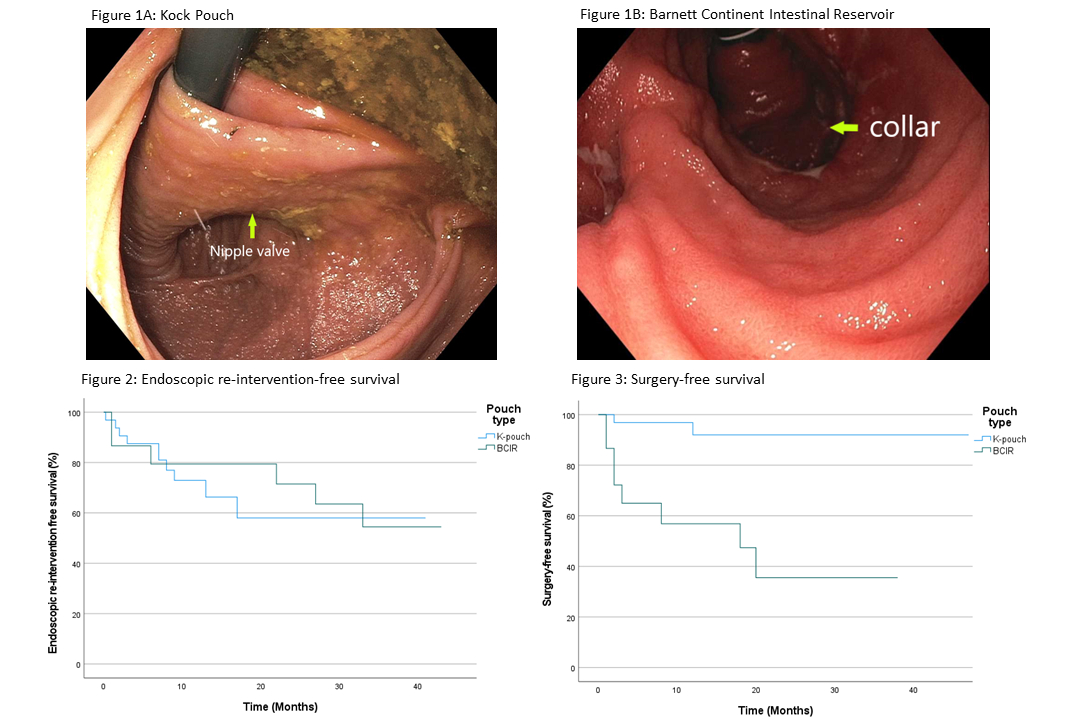
All consecutive eligible patients with a continent ileostomy who underwent an endoscopic procedure, between 2019 and 2023 were evaluated through an IRB-approved registry at the Center for Ileal Pouch Disorders of Columbia University Irving Medical Center/New York Presbyterian Hospital. Primary outcomes were CI corrective surgery-free survival (without revision or conversion) and endoscopy-reintervention-free survival. Secondary outcomes were the presence of pouch disorders and the requirement for endoscopic and medical therapy.
Results
A total of 49 patients were included with a mean age of 57.1±15.2 years and predominantly being females (N=39, 79.5%). Thirty-two patients (65.3%) had a K-pouch and 17 (34.7%) had a BCIR. The median follow-up for the whole cohort was 17.0 months (IQR=23.0). Demographic and clinical data are listed in Table. There are no significant differences in demographic characteristics, underlying diagnosis, the indication for colectomy and CI, and current medications between the two groups. However, the urgency for intubation of the CI was more common (5, 29.4%) in the BCIR group than in the K-pouch group (2, 6.2%) (P=0.02). There were no statistical differences in structural and inflammatory disorders on endoscopy and associated endoscopic treatment modalities between the two groups. Twelve (24.4%) patients reported on the efficacy of therapy, with 9 (75.0%) experiencing symptom improvement (Table). Over the follow-up period, patients in the BCIR group required more surgical intervention than those in the K-pouch group (P< 0.001), with the surgery-free survival for the BCIR group being 18.8±4.3 compared to 43.8±2.1 in the K-pouch group (P<0.001) (Figure 3). Sixteen (32.6%) patients required endoscopic re-intervention, 10 (31.2%) were in the K-pouch group, and 6 (35.2%) in the BCIR group (P=0.7) (Figure 2). None of the patients underwent conversion to a permanent stoma (i.e. Pouch failure).
Conclusions:
The incidence of pouch failure in continent ileostomy appears to be low. Our findings suggest that K-pouch may provide better short and long-term outcomes than BCIR.