Introduction: Hemorrhoidal disease is very common in the U.S. with self-reported incidence of 10 million per year. A broad range of interventions exist to address symptomatic hemorrhoids from rubber band ligation and sclerotherapy to excisional hemorrhoidectomy or stapled hemorrhoidopexy. Several studies have shown advantages of stapled hemorrhoidopexy including decreased post-operative pain and shorter hospital stay; however, articles focusing on long-term results have described higher rates of recurrence compared to excision along with serious complications including rectovaginal fistula, pelvis sepsis, rectal perforation, and acute rectal obstruction.
Case Presentation: A 62-year-old female presented with a 4-day history of stool per vagina 12 days after stapled hemorrhoidopexy for treatment of prolapsed hemorrhoids. A CT scan showed an air-filled vaginal cuff with loss of plane between the rectum and vagina concerning for rectovaginal fistula. Preoperative workup included exam under anesthesia, and a full-thickness 0.5-0.75cm anterior rectal defect was noted at 4-5cm above the anal verge without any significant surrounding inflammation or evidence of infection. Given the significant disruption of the rectovaginal septum, it was determined a transperineal approach with muscle interposition and proximal diversion would be the most ideal option in order to give the patient the highest likelihood of durable repair. Thus, a multidisciplinary approach with the plastic surgery and colorectal teams was employed. The patient underwent both mechanical and antibiotic bowel preparations. The fistula tract was identified with a fistula probe with dissection of rectum from vagina. Both the vaginal and rectal defects were closed primarily. The plastic surgeon harvested a left gracilis flap for interposition. Finally, a laparoscopic diverting loop ileostomy was created. The patient was admitted and placed on bedrest for 48 hours postoperatively and was not allowed to sit upright for 2 weeks. This was followed by slowly incorporating sitting three times a day with plans to liberate activity restrictions at the plastic surgeonís discretion. The perineal drain was removed, and she was discharged on post operative day 4.
Discussion: Stapled hemorrhoidopexy appears to be at least as safe as excisional hemorrhoidectomy with meta-analyses showing no significant difference in overall postoperative complications. Rectovaginal fistula incidence after the stapled technique has rarely been noted in case reports with estimated incidence of about 0.2%. Primary fistula repair alone has been associated with lower success rates compared to combined procedures with interposition of healthy, vascularized tissue. A gracilis muscle flap interposition can serve as a viable option for such a repair in treatment of this complex, albeit rare, complication of stapled hemorrhoidopexy.
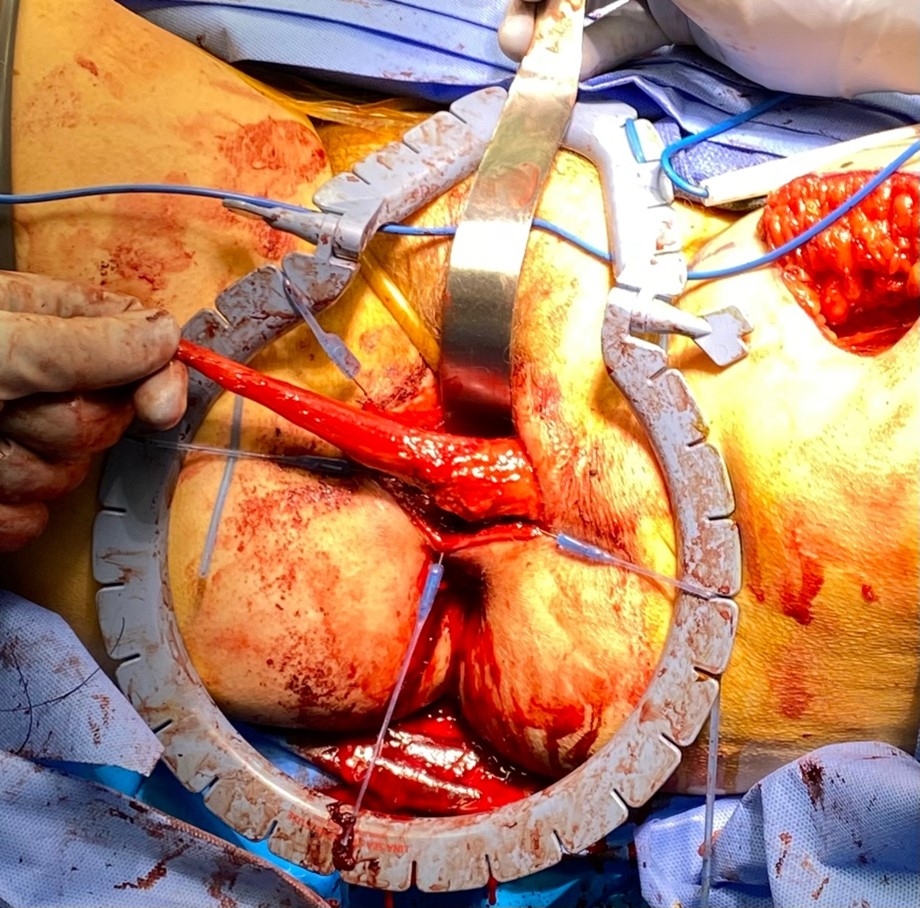
Transperineal incision with rectal and vaginal defects closed, left gracilis interposed