Background and aim:
Solitary rectal ulcer syndrome (SRUS) is an uncommon benign disorder. Macroscopically, SRUS can be classified into ulcerative, polypoidal, and flat types. Patient education and behavior modification are the mainstay lines of treatment. Yet, surgery is recommended for refractory cases, nonetheless, is not shown to be beneficial in most patients and may lead to catastrophes. Endoscopic procedures including sclerotherapy, human fibrin sealant, botulinum toxin and trial for endoscopic mucosectomy were previously reported. Nonetheless, no previous trials for endoscopic submucosal dissection (ESD) for SRUS were published to the best of our knowledge. We aimed in this study to explore the feasibility, efficacy, and outcome of ESD for solitary rectal ulcer syndrome.
Methods:
In this retrospective observational single-center study, patients who underwent ESD between January 2021 and October 2023, with the final diagnosis as SRUS, were included. Patientsí medical records were recruited, and data including baseline demographics, endoscopic findings, procedure duration, technical and clinical success, adverse events and follow up duration were recorded.
Results:
A total of 7 patients (5 males, median age: 18y (range: 14-63y)) were enrolled in the current study. All patients presented with bleeding per rectum. Primary endoscopy revealed polypoidal rectal lesions of variable size (median: 8cm, range:5-13.5cm) with superficial ulcerations in most cases. Initial pathology revealed ulcerated adenomatous lesion with low grade dysplasia (LGD) (71.4%), ulcerated hyperplastic polyp or inflammatory hamartomatous polyp in the remaining patients. Technical success was achieved in all patients within a median time (180 minutes) using either tunnelling, bridging or mucosal flap traction ESD technique. No procedure related adverse events were recorded except delayed bleeding in one case which was controlled with conservative measures. All patients showed marked clinical improvement with stoppage of bleeding. Delayed adverse events included narrowing of the rectal lumen necessitating balloon dilatation in one patient. Final pathological analysis revealed a final diagnosis of SRUS with no dysplasia (57.1%), with LGD (28.6%) and with foci of high-grade dysplasia (14.3%). Follow up endoscopy was done in 74.1% of patients at median timing (6 months, range: 4-18 months) revealing no recurrence of polypoidal lesions in all patients. However, non-bleeding ulcers were present in 60% of patients. Defecography revealed pelvic floor dysfunction in 80% of patients.
Conclusion:
ESD was shown to be a feasible, safe and effective technique for the management of SRUS (polypoidal type) with hopeful outcome.
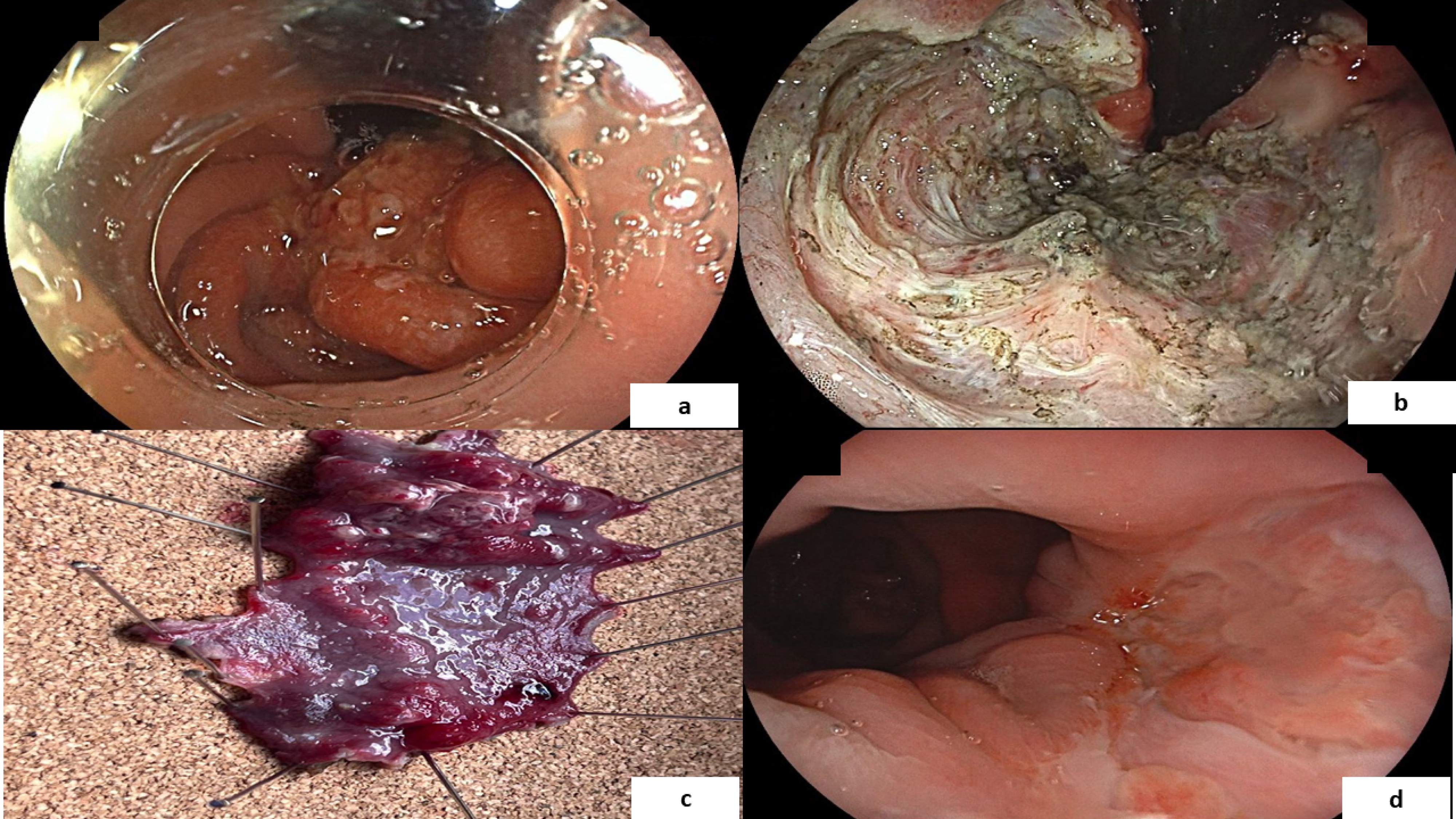
Endoscopic image of solitary rectal ulcer showing multiple rectal polypoidal ulcerated lesions (a), view after complete enbloc resection (a), pathological specimen (c). Follow up endoscopy few months later showing small rectal ulcers with no recurrence of polypoidal lesions.
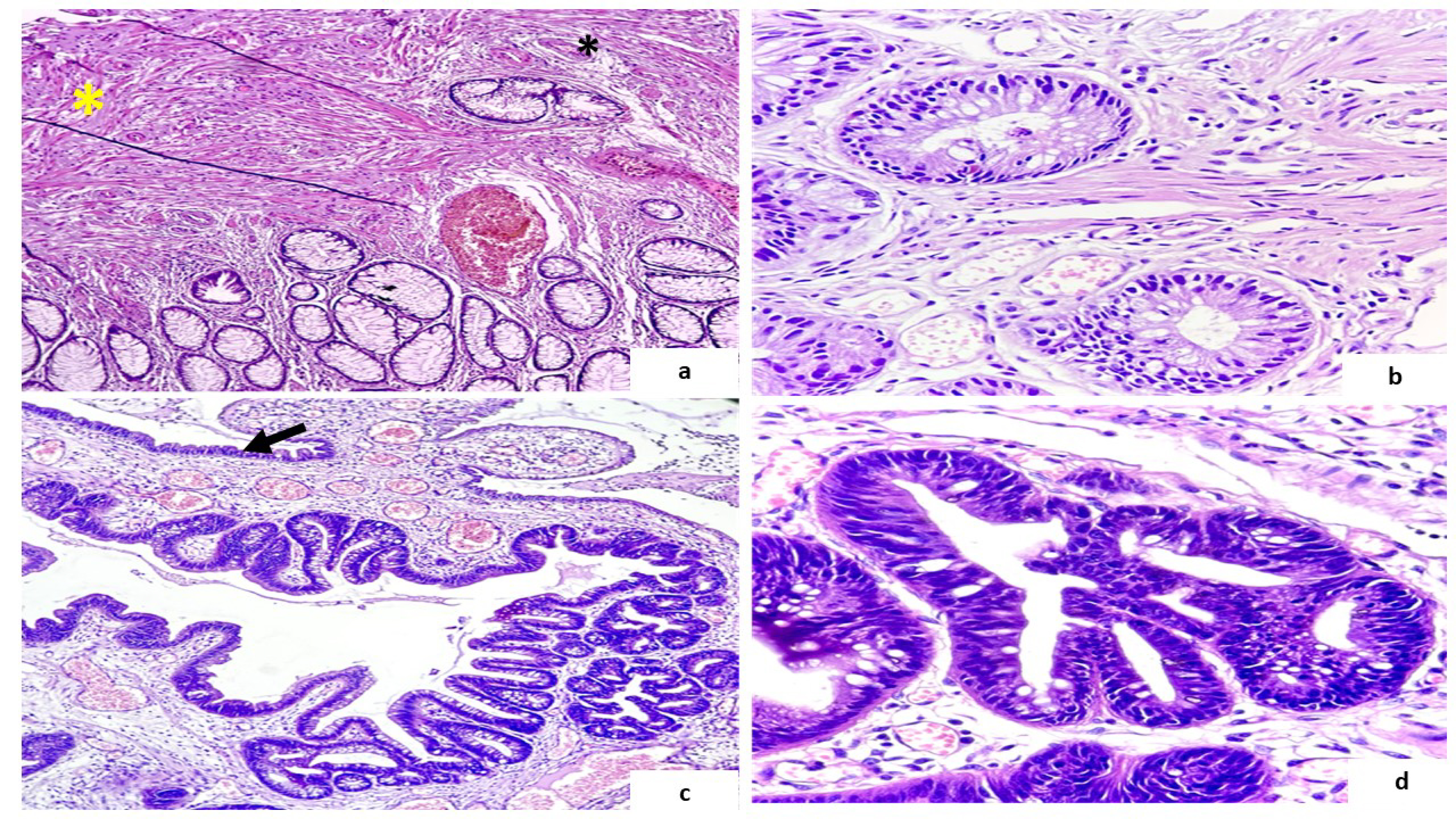
Photomicrographs of ESD of solitary rectal ulcer specimen showing ulcerated surface (arrow), thickened muscularis mucosa with splayed fibers in-between mucosal crypts (Asterix) (a) and (b). An occasional focus of low-grade dysplasia in (c) and (d). [H&E stain, Original magnification 40, x100, x100, x400 respectively]