Background
Sarcopenia has been recognised as a determining factor in the success of surgery and is associated with an increased risk of postoperative complications and readmission. Diagnosis is currently based on clinical guidelines, which includes assessment of skeletal muscle mass but not quality. Ultrasound has been proposed as a useful point-of-care diagnostic tool to assess muscle quality, but no validated cut-offs for sarcopenia have been reported. The use of a novel automated artificial intelligence (AI) software to interpret ultrasound images may help mitigate the operator-dependent nature of the modality. Our study aims to validate the use of AI-aided ultrasound as a reliable and reproducible way to assess muscle quality and diagnose sarcopenia.
Methods
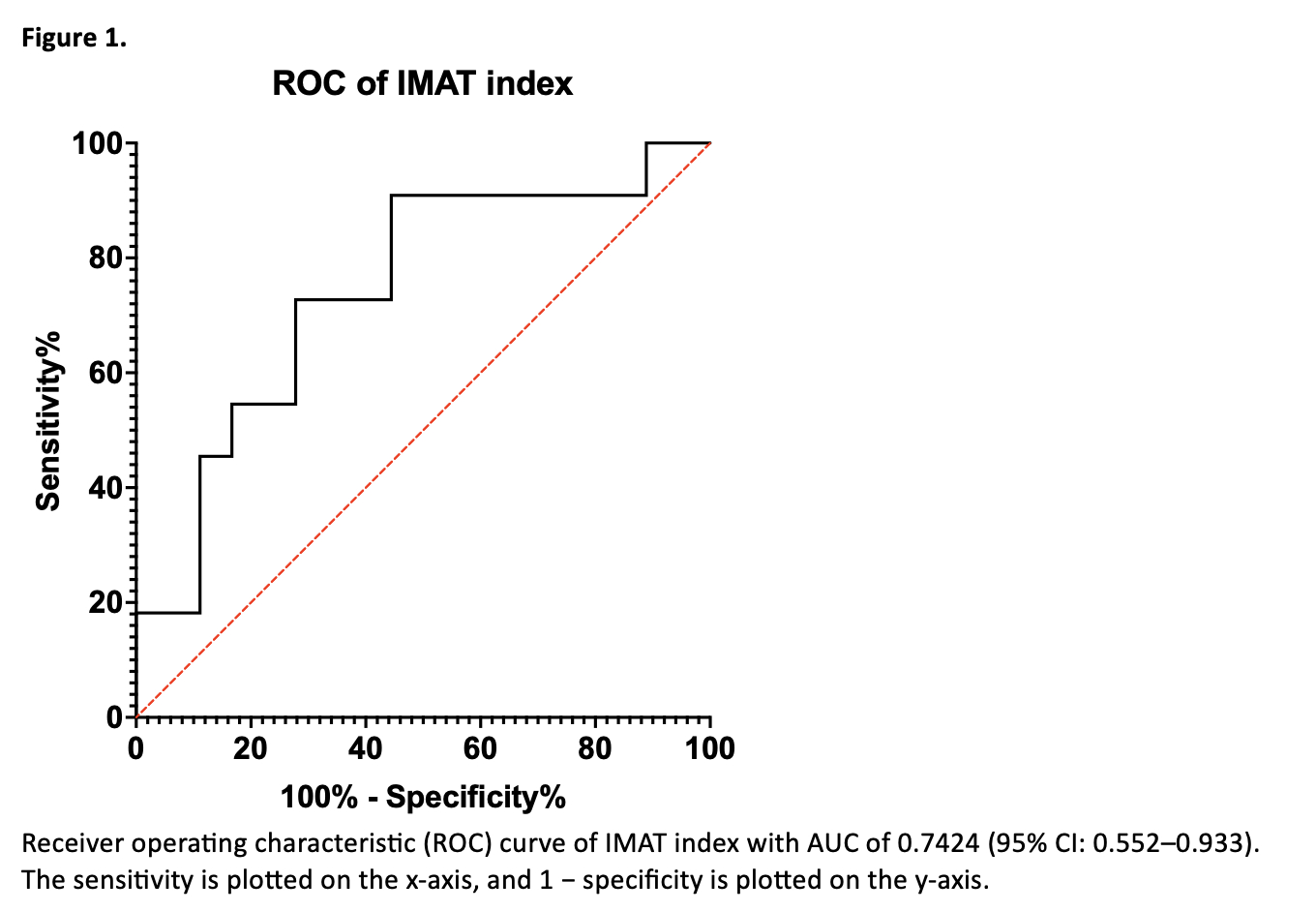
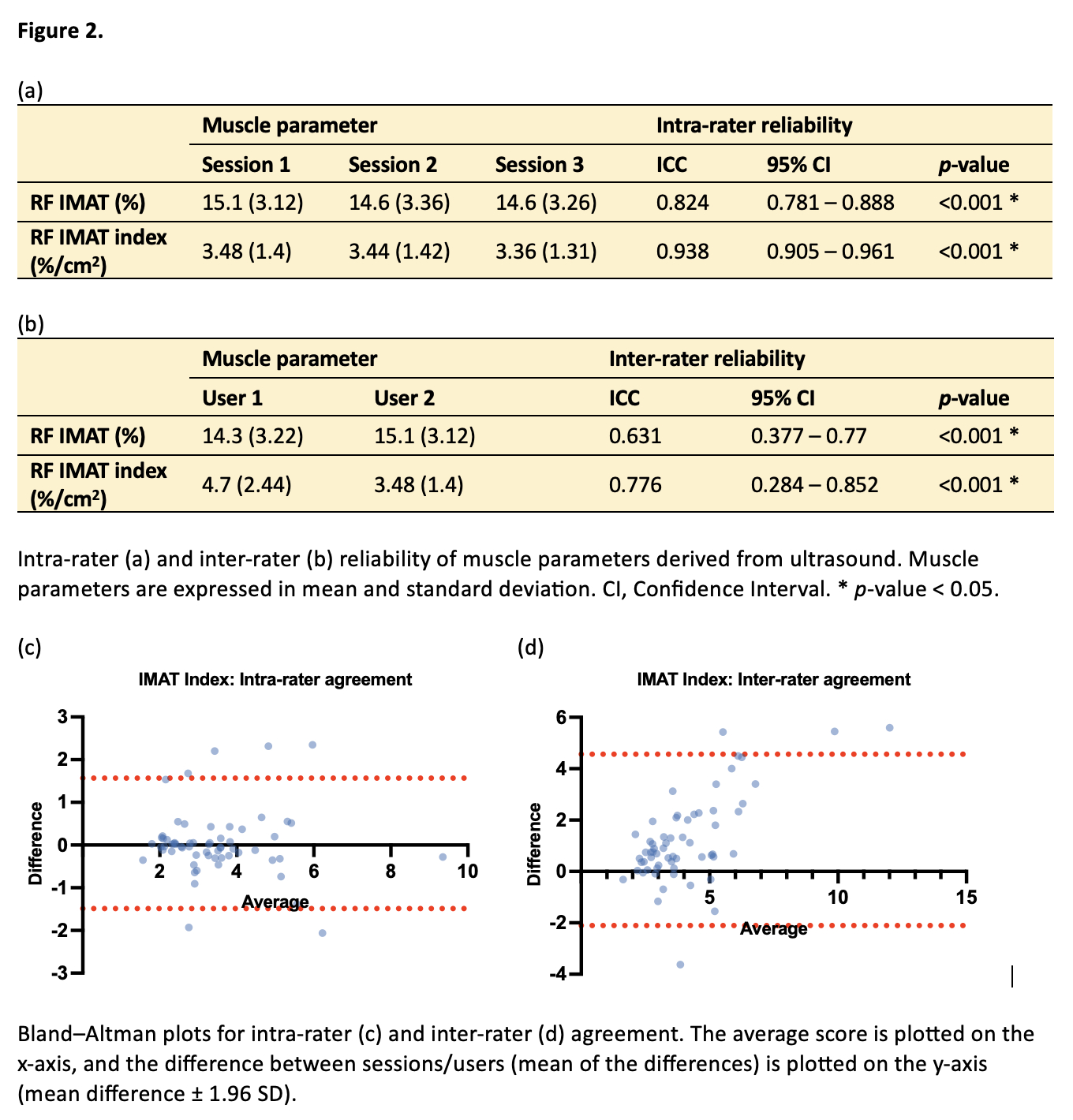
Adult participants from the outpatient clinic were recruited for this prospective cohort study. Sarcopenia was diagnosed according to the Asian Working Group for Sarcopenia (AWGS) 2019 guidelines. Ultrasonography of the participants’ rectus femoris muscle was performed and the images were analysed by an AI software to derive muscle parameters, including intramuscular adipose tissue (IMAT) as a proxy of muscle quality. A receiver operative characteristic (ROC) curve was used to assess the predictive capability of IMAT and its derivatives, with area under the curve (AUC) as a measure of overall diagnostic accuracy. Intra- and inter-rater reliability of muscle ultrasound parameters was analysed in a separate cohort using intraclass correlation coefficients (ICC) and Bland-Altman plots.
Results
29 participants were included in the interim analysis. The median age was 71 years (range: 26-87) and prevalence of sarcopenia in the cohort was 37.9%. The ROC curve plotted with IMAT index (IMAT% divided by muscle area) yielded an AUC of 0.7424 (95% CI: 0.552–0.933) (Fig 1). An optimal cut-off point of 3.835%/cm2 for IMAT index was determined with a Youden’s Index of 0.465. IMAT index has excellent intra-rater reliability (ICC = 0.938, CI: 0.905–0.961) and good inter-rater reliability (ICC = 0.776, CI: 0.627–0.866). In Bland-Altman plots, the limits of agreement were -1.489 to 1.566 and -2.107 to 4.562 respectively (Fig 2).
Discussion
IMAT index derived from ultrasound has the potential to be an alternative tool for sarcopenia screening and diagnosis, with good intra- and inter-rater reliability. The proposed IMAT index cut-off maximises sensitivity for case finding, making it useful as a point-of-care test in the community and enabling earlier intervention. AI-aided ultrasound can also be used to track patients’ progress and muscle quality through various stages of treatment, such as the pre-, peri-, and post-operative period for surgical patients. Further analysis incorporating other ultrasound parameters of muscle quality may provide the basis for a more robust diagnostic tool when the study is completed.